➲ Home ➲ C-19 Archives
📖 Does Covid Lead to Dementia? What We Know About Covid’s Impact on Your Brain
‘For patients already battling Alzheimer’s disease, studies indicate that Covid can exacerbate brain inflammation, damage immune cells, and accelerate the disease.
Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection.
Mild Covid cases in younger adults have also been linked to brain issues affecting memory and thinking.’
📖 (3 Mar 2025 ~ Bloomberg UK) ‘What We Know About Covid’s Impact on Your Brain’.
© 2025 Jason Gale / Bloomberg UK.
❦ Financial media article ~ ‘What We Know About Covid’s Impact on Your Brain’
By Jason Gale / Bloomberg UK (3 Mar 2025)
❦ ‘Five years after the pandemic began, researchers are increasingly recognizing the toll Covid can take on brain health.
Many of those who have had the disease struggle with persistent issues such as brain fog, depression and cognitive slowing, hindering their ability to work and otherwise function.
Scientists have found that those who have had Covid are more likely to have elevated levels in their blood of the same proteins that are prevalent in people with Alzheimer’s disease.
Researchers are concerned that the findings could be early warning signs of a future surge in cases of dementia and other neurodegenerative conditions, prolonging Covid’s societal, economic, and health burden.
❦ What do studies show about Covid and the brain?
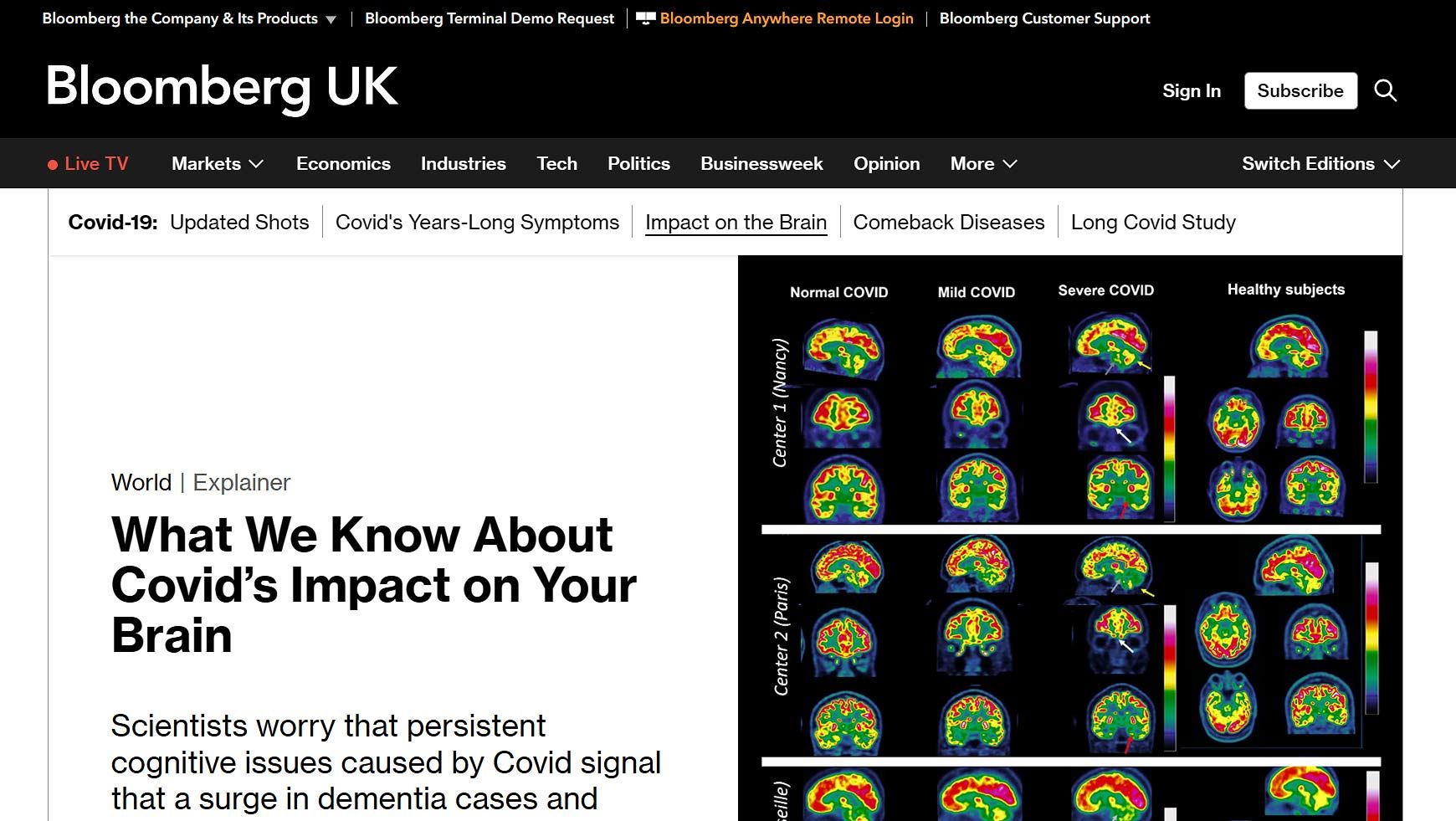
In 2021, UK researchers reported early results from a study comparing brain scans taken before and after the pandemic began.
They discovered signs of damage and accelerated aging in the brain, particularly in the part responsible for smell – even in patients who had experienced mild cases of Covid months earlier.
Research has since shown that Covid-related cognitive deficits can persist for years, especially in older adults and those who suffered from more severe cases.
For instance, a study of people aged 60 or older who were hospitalized during China’s first Covid wave showed that 2 1/2 years later, 40% developed cognitive impairment, compared with just 14% of their uninfected spouses.
A 2024 UK study of people hospitalized for Covid treatment concluded that as a group they showed a significant worsening of psychiatric and cognitive symptoms two to three years after their discharge.
At that stage, half experienced moderate to severe depression, a quarter suffered severe cognitive decline, and one in nine showed a loss of mental function equivalent to a 30-point drop on the IQ scale, where a score of 100 is average.
‘For patients already battling Alzheimer’s disease, studies indicate that Covid can exacerbate brain inflammation, damage immune cells, and accelerate the disease.
Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection.’
For patients already battling Alzheimer’s disease, studies indicate that Covid can exacerbate brain inflammation, damage immune cells, and accelerate the disease.
Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection. Mild Covid cases in younger adults have also been linked to brain issues affecting memory and thinking.
These symptoms typically fluctuate and tend to worsen after physical or mental exertion, often impairing the ability of individuals to work and socialize.
A February 2024 study of nearly 113,000 people found greater loss of memory and executive function among people who had been infected at some point by the SARS-CoV-2 virus that causes Covid compared with those who had never had it.
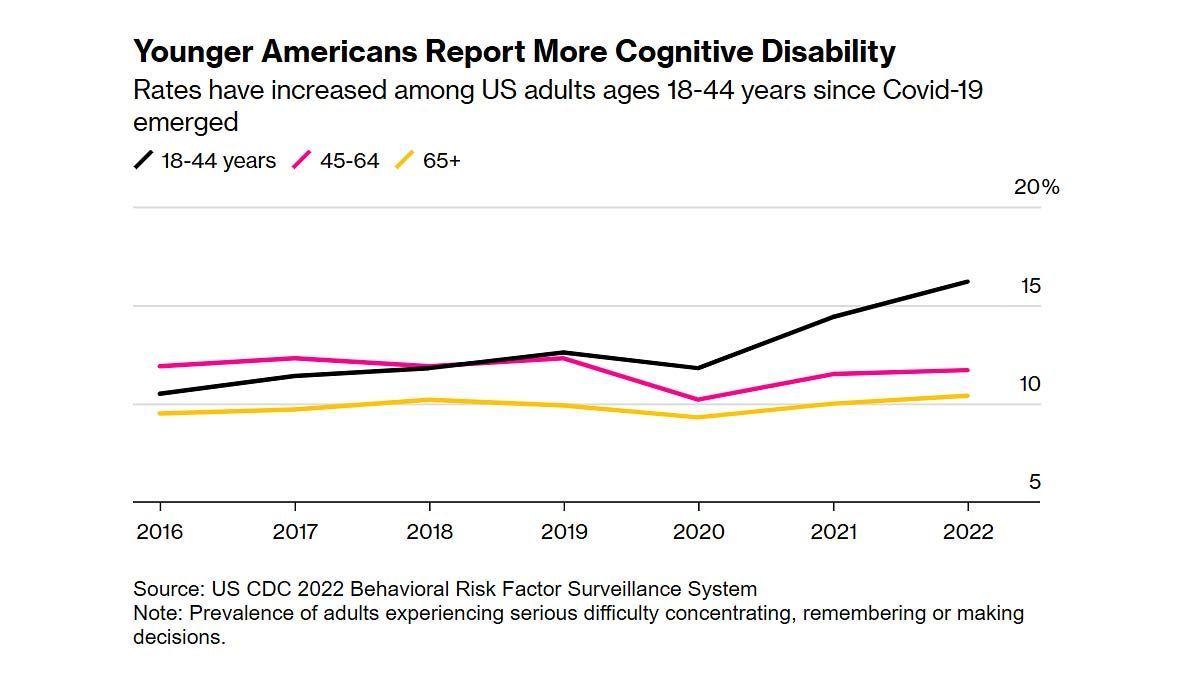
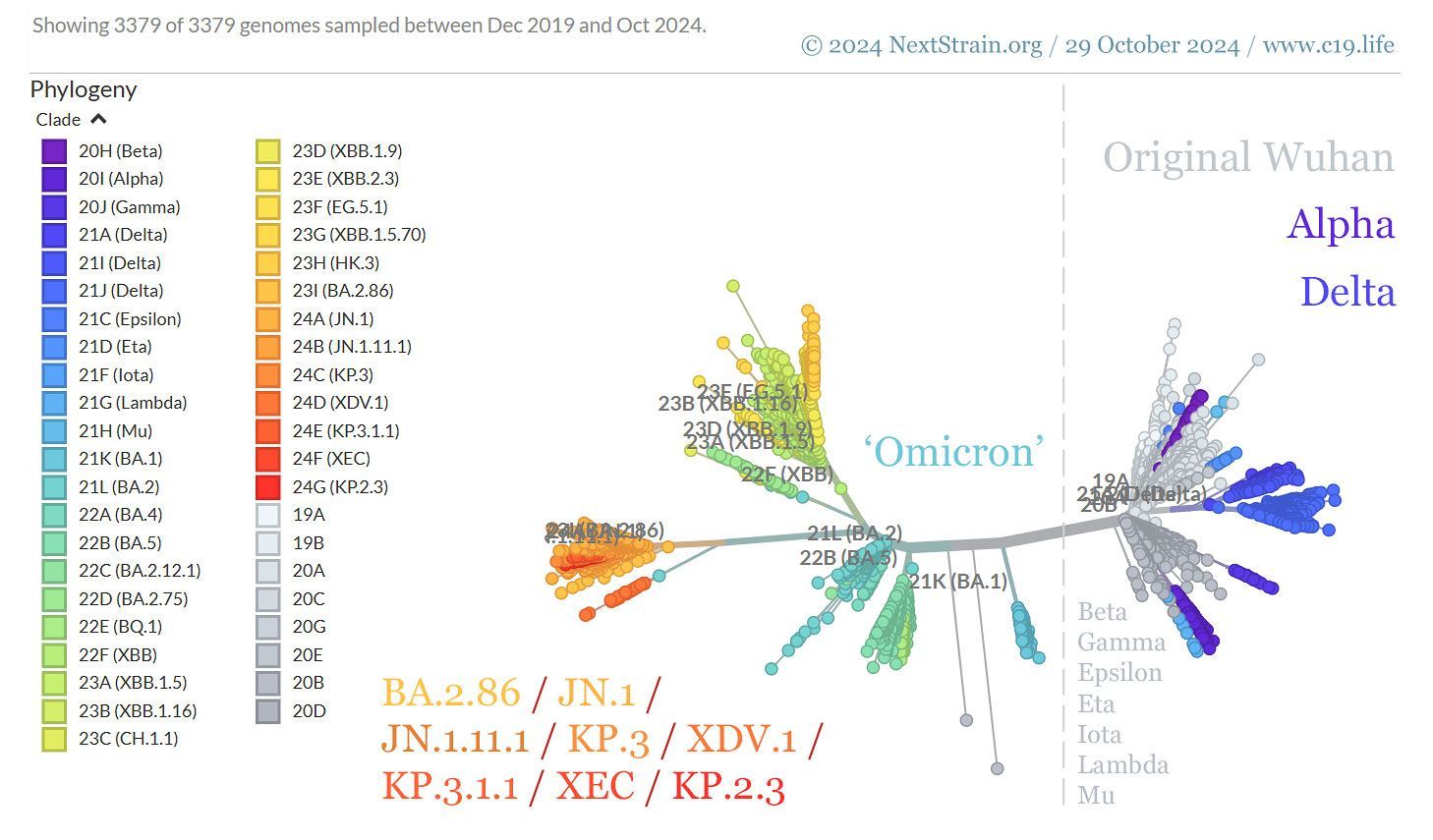
People who were struck later in the pandemic had smaller deficits compared with those infected with either the original or the alpha strain, the first variant of the virus to come to researchers’ attention.
‘The same study found that even mild cases of Covid led to cognitive decline, equivalent to an average 3-point drop in IQ.
For those with unresolved symptoms such as persistent shortness of breath or fatigue, the decline amounted to a 6-point decrease in IQ.’
UK scientists reported subtle but persistent cognitive effects in a so-called human challenge study published in September 2024.
For the research, 34 healthy volunteers ages 18 to 30 completed 11 tasks on an iPad during two consecutive days before they were deliberately exposed to the original SARS-CoV-2 strain.
Roughly half the group developed an infection. None of the participants noticed any cognitive effects after their initial exposure to the coronavirus.
‘However, six further rounds of testing found the infected group had measurable reductions in memory and executive function compared with those who weren’t infected, with the differences still evident a year after the experiment.’
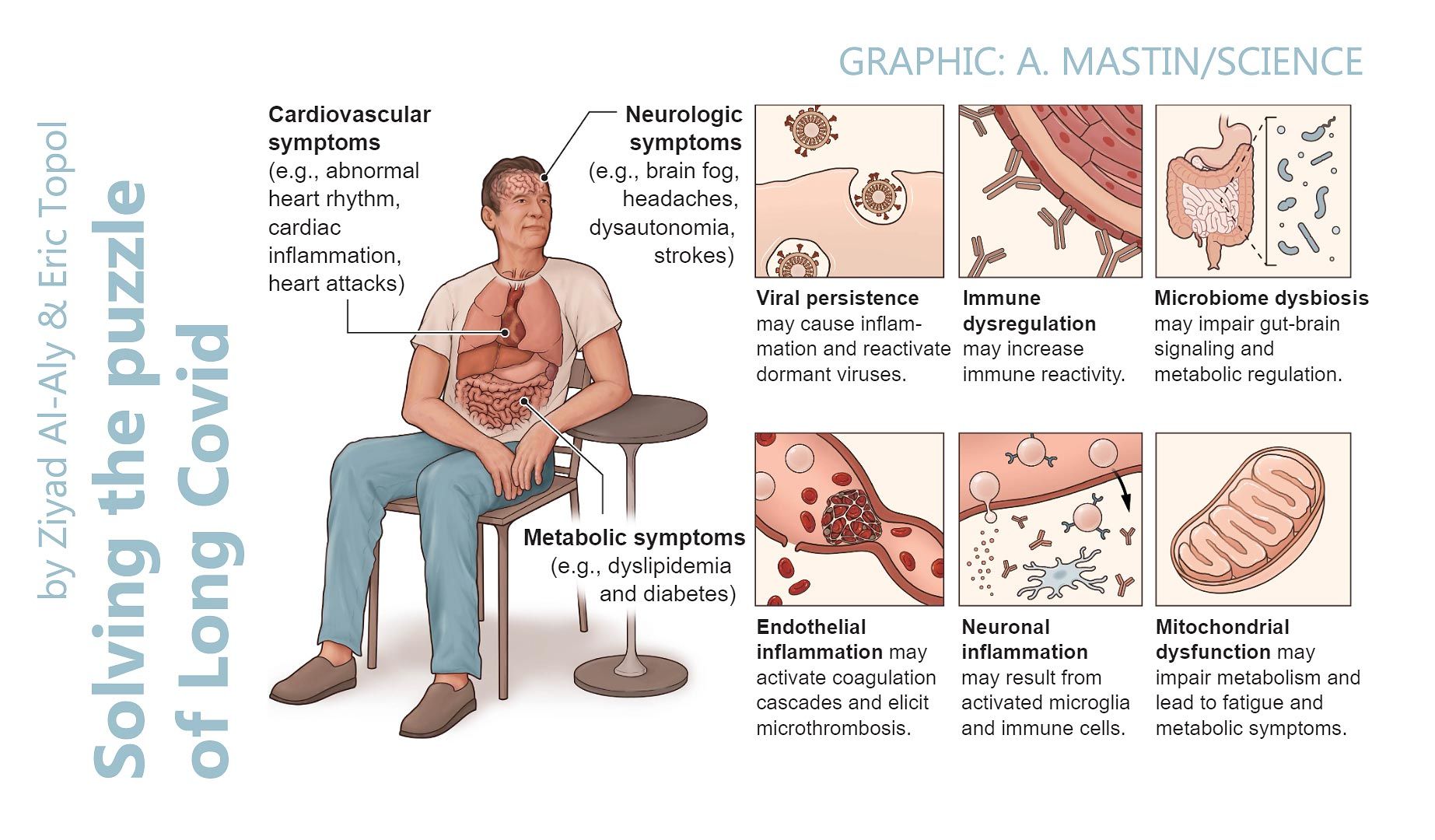
Studies also suggest that neurological and neurocognitive symptoms – such as headaches, confusion, and brain fog – may be more common among female long Covid patients than their male counterparts, highlighting potential sex-based differences in the virus’s long-term impact on the brain.
Some evidence suggests an infection may increase the risk of Parkinson’s disease.
This link is supported by the rise in cases of parkinsonism – a collection of symptoms such as tremors, slow movement, stiffness and balance issues – following a case of Covid.
❦ How many people are affected?
There is no robust global data on the number of people experiencing prolonged neurocognitive symptoms after a bout of Covid.
A 2022 population-based study in the Netherlands estimated that long Covid affects about one in eight people after infection, with vaccination only partially reducing the risk.
By 2024, the condition was estimated to have afflicted around 400 million people worldwide, with brain fog as a primary symptom.
While some people recover over time, a 2025 study found about 4.5% of infected adults may develop myalgic encephalomyelitis (also known as chronic fatigue syndrome), a debilitating and often long-term condition characterized by worsening symptoms after physical or mental exertion, unrefreshing sleep, and either cognitive impairment or dizziness when standing.
Different studies have found that anywhere from 7% to 59% of people still have problems with thinking and memory three months after recovering from Covid, according to one review of the research.
❦ How does Covid harm the brain?
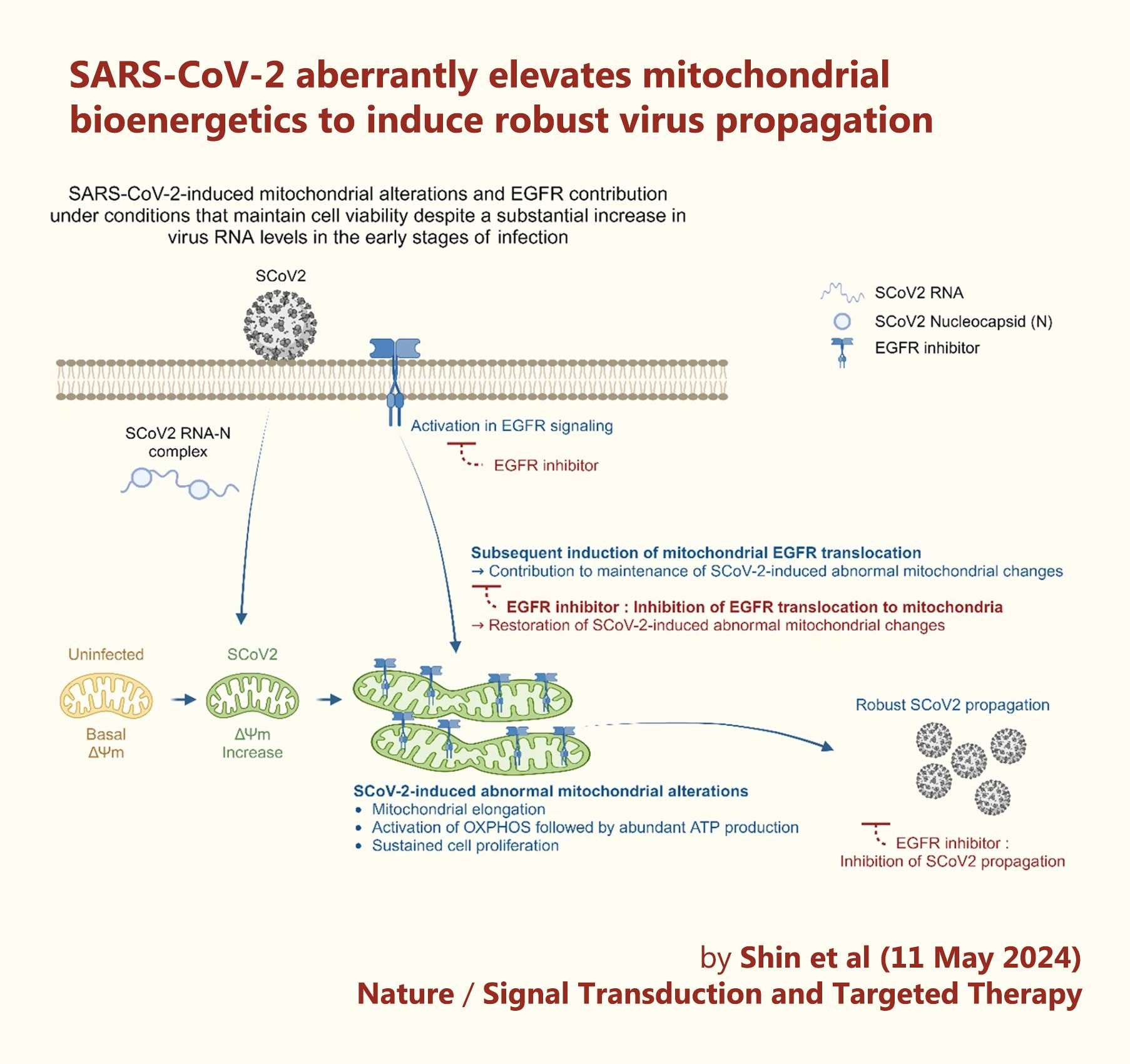
The effects of a SARS-CoV-2 infection on the brain are the focus of intense research and remain only partially understood.
A study published in January by scientists at Imperial College London found that Covid survivors were more likely to have elevated levels of beta amyloid and tau-181 – proteins linked to Alzheimer’s disease – in their blood.
These findings suggest that a case of Covid could heighten the future risk of developing the disease.
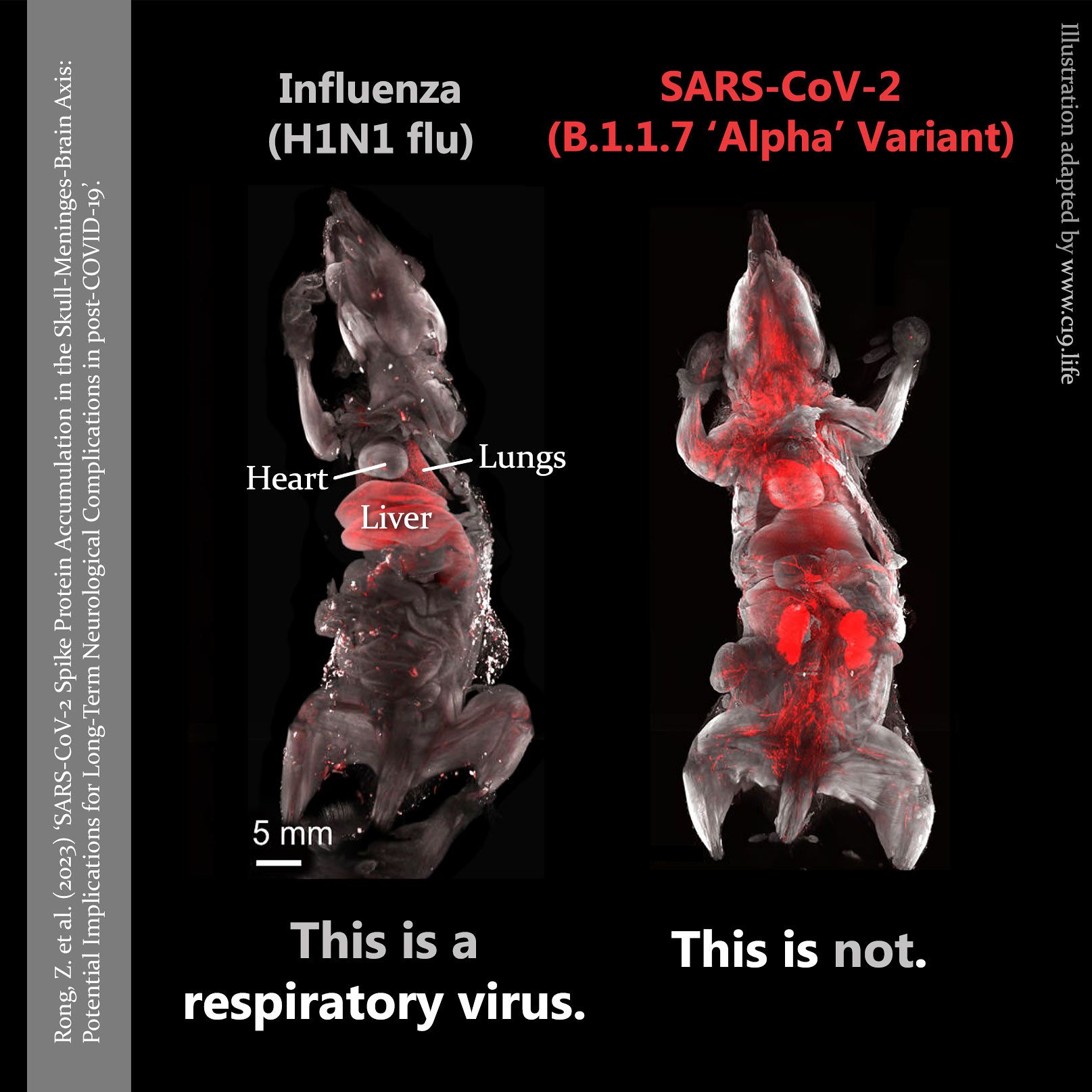
Other studies suggest that during acute infection, the virus may damage nerves, particularly in the olfactory bulb – which transmits smell impulses to the brain.
This damage could lead to long-lasting issues, with the virus potentially infecting the brain through this pathway, altering its structure and resulting in impaired cognition and fatigue.
Persistent viral remnants or the initial infection itself may trigger neuroinflammation and disrupt the immune system, causing antibodies and T cells to mistakenly attack healthy brain cells, damage blood vessels, and harm the blood-brain barrier.
A study published in late 2024 found that the virus’s spike protein can linger in the body for years after infection, particularly in areas around the skull and brain, potentially contributing to the neurological symptoms of long Covid.
Additional research points to blood clots as potential drivers of damage to nerve cells and restricted oxygen and nutrient supply to the brain.
A SARS-CoV-2 infection during pregnancy – particularly in mothers who were unvaccinated or had no prior infection – may also increase the risk of neurodevelopmental delays in their offspring, though scientists are still working to understand the extent of this risk amid inconsistent findings.
❦ What is the possible economic impact?
While the long-term effects of Covid on conditions such as Parkinson’s disease and dementia remain uncertain, the stakes are high.
These are both lifelong, incurable, progressive illnesses with a profound societal impact, affecting not only those diagnosed but also their families, caregivers and the broader healthcare system.
Already, there are significant economic repercussions globally from the enduring prevalence of long Covid. Analysts have put the annual economic toll at between $864 billion and $1.04 trillion in developed nations alone – roughly 1% of the global economy.
Much of the impact stems from on-going disability and illness, with persistent fatigue and concentration problems among the most common conditions.
‘Long Covid has
disproportionately affected younger adults in their prime.’
Long Covid has disproportionately affected younger adults in their prime – those who drive much of the workforce, productivity and innovation – exacerbating labor shortages and straining economic growth.’
❂
❦ Related information
- Related explainers on long Covid and Covid vaccine safety.
- Neurologists Serena Spudich and Avindra Nath outline the nervous system consequences of Covid.
- Neurologist Michelle Monje talks about the effects of long Covid on the brain.
- Epidemiologist Ziyad Al-Aly discusses how Covid leaves its mark, and global biosecurity expert Raina MacIntyre and colleagues look at its after-effects in Australia.
❂
📖 (3 Mar 2025 ~ Bloomberg UK) ‘What We Know About Covid’s Impact on Your Brain’.
© 2025
Jason Gale
/
Bloomberg UK.
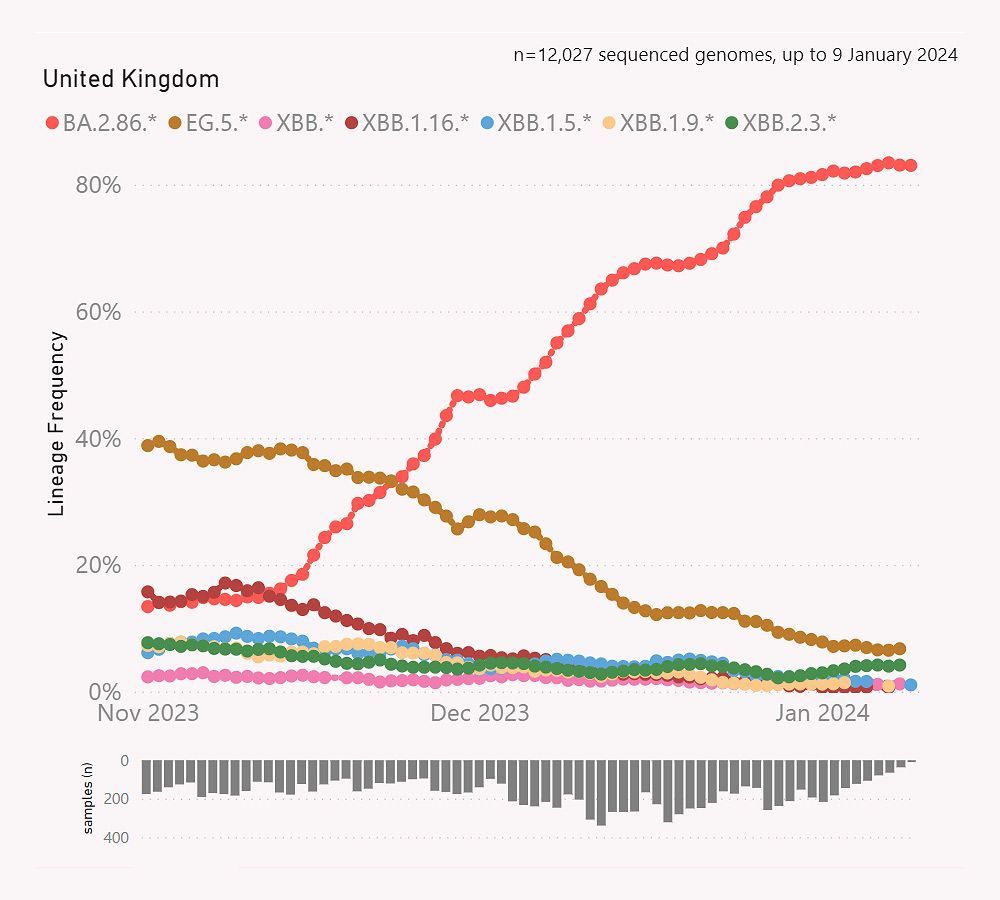
Legend: ‘Younger Americans Report More Cognitive Disability’.
‘Prevalence of adults experiencing serious difficulty concentrating, remembering, or making decisions.
Rates have increased among US adults ages 18-44 years since Covid-19 emerged.’ ➤
📖 (3 Mar 2025 ~ Bloomberg UK) What We Know About Covid’s Impact on Your Brain ➤
© 2025 Image Source: US CDC 2022 Behavioral Risk Factor Surveillance System.
❂
More... Dementia & the Brain
More... PASC (‘Long Covid’)
C-19: Archives
Useful search tags:
air filtration / babies & children / body / brain / C19.Life / cancer / comment / dementia / economy / elders / excess deaths / exercise / flu / heart / history / hospitals / immunity / influenza / law / Lisa Iannattone / long covid / lungs / mitochondria / muscles / musculoskeletal / NHS / Noor Bari / nosocomial / PEM / parkinson’s / propaganda / reinfections / reproduction and pregnancy / resources / respirators / respiratory / risk / SARS(-CoV-1) / schools / solutions / transmission / universities / UVC / vaccines / variants / WHO / young adults / zoonosis