by Florence Nightingale (1859/1860)
•
19 February 2024
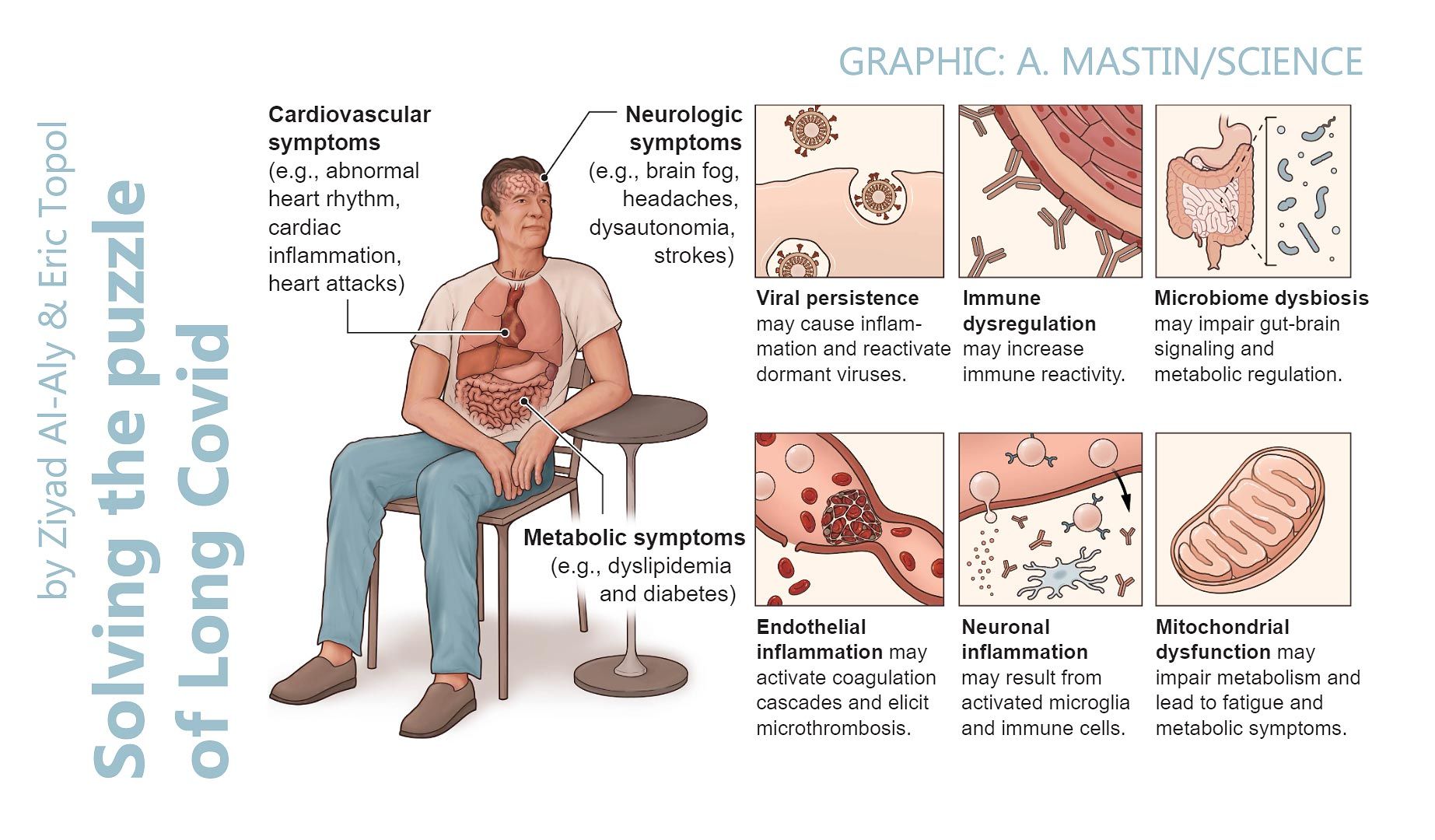
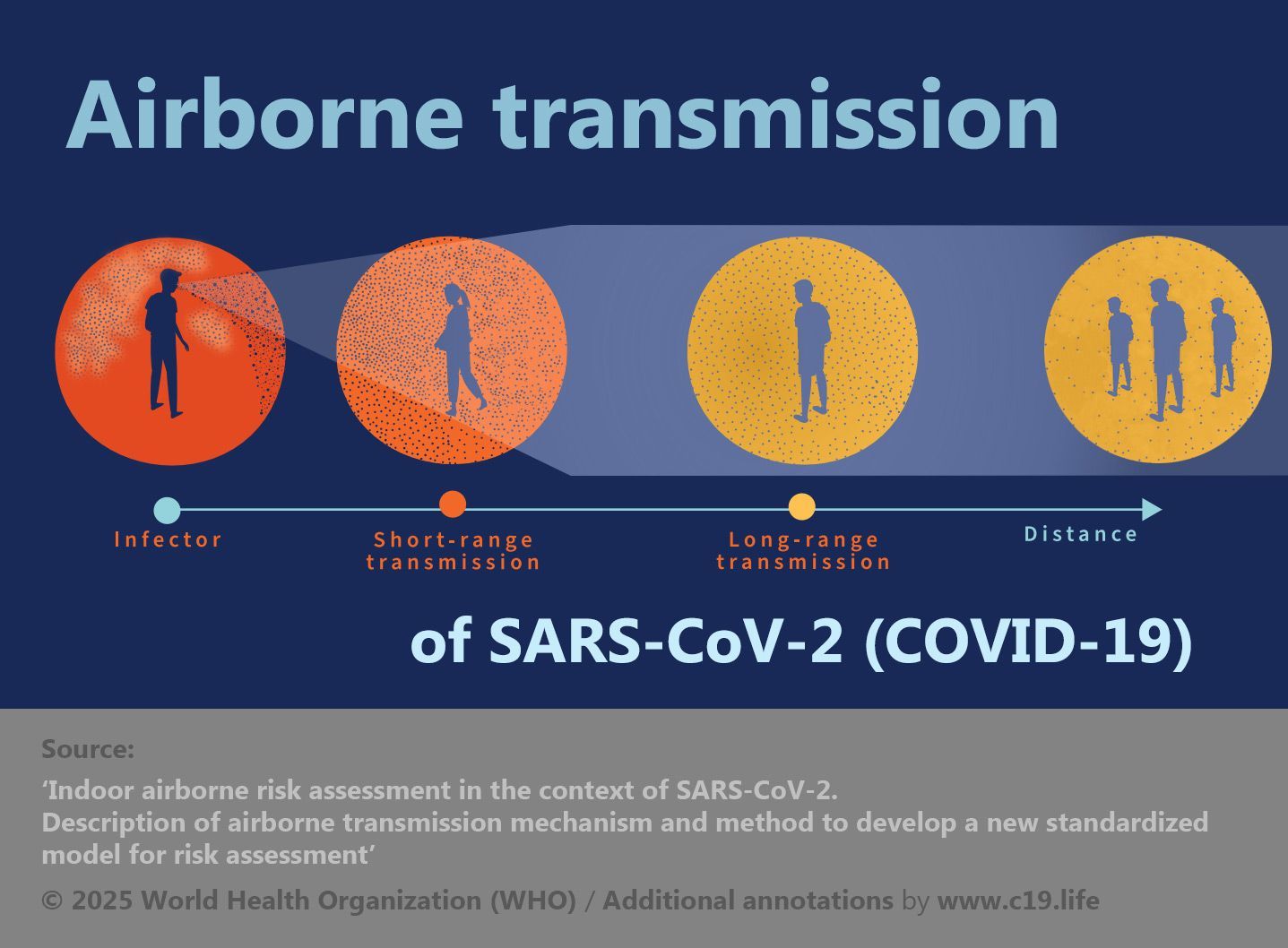
‘The very first canon of nursing... the first essential to the patient... is this: to keep the air he breathes as pure as the external air, without chilling him .’ ❂ Notes on Nursing (1860 edition) By Florence Nightingale First Published 1859. Revised edition reprinted in 1860 by Harrison of Pall Mall Accessed 19 Feb 2024 ❦ Chapter I – Ventilation and Warming ‘The very first canon of nursing, the first and the last thing upon which a nurse’s attention must be fixed, the first essential to the patient, without which all the rest you can do for him is as nothing, with which I had almost said you may leave all the rest alone, is this: TO KEEP THE AIR HE BREATHES AS PURE AS THE EXTERNAL AIR, WITHOUT CHILLING HIM. Yet what is so little attended to? Even where it is thought of at all, the most extraordinary misconceptions reign about it. Even in admitting air into the patient’s room or ward, few people ever think where that air comes from. It may come from a corridor into which other wards are ventilated, from a hall, always unaired, always full of the fumes of gas, dinner, of various kinds of mustiness; from an underground kitchen, sink, wash-house, water-closet, or even, as I myself have had sorrowful experience, from open sewers loaded with filth; and with this the patient’s room or ward is aired, as it is called – poisoned, it should rather be said. Always air from the air without, and that, too, through those windows, through which the air comes freshest. From a closed court, especially if the wind do not blow that way, air may come as stagnant as any from a hall or corridor. I know an intelligent humane house surgeon who makes a practice of keeping the ward windows open. The physicians and surgeons invariably close them while going their rounds; and the house surgeon, very properly, as invariably opens them whenever the doctors have turned their backs. I have known a medical officer keep his ward windows hermetically closed, thus exposing the sick to all the dangers of an infected atmosphere, because he was afraid that, by admitting fresh air, the temperature of the ward would be too much lowered. This is a destructive fallacy. To attempt to keep a ward warm at the expense of making the sick repeatedly breathe their own hot, humid, putrescing atmosphere is a certain way to delay recovery or to destroy life.’ ❂ ‘I have known cases of hospital pyæmia quite as severe in handsome private houses as in any of the worst hospitals, and from the same cause, viz., foul air. Yet nobody learnt the lesson. Nobody learnt anything at all from it.’ ❂ ✪ C-19: On schools ‘Of all places, public or private schools, where a number of children or young persons sleep in the same dormitory * , require this test of freshness to be constantly applied.’ * [ C-19 Note: You might substitute ‘sleep’ and ‘dormitory’ with ‘study’ and ‘classroom’ in this section.] ‘If it be hazardous for two children to sleep together in an unventilated bedroom, it is more than doubly so to have four, and much more than trebly so to have six under the same circumstances. People rarely remember this; yet, if parents were as solicitous about the air of school bedrooms as they are about the food the children are to eat, and the kind of education they are to receive, at school, depend upon it due attention would be bestowed on this vitally important matter, and they would cease to have their children sent home either ill, or because scarlet fever or some other “current contagion” had broken out in the school. There are schools where attention is paid to these things, and where “children’s epidemics” are unknown.’ ❂ ✪ C-19: Offices, shops, factories, and other workplaces ‘How much sickness, death, and misery are produced by the present state of many factories, warehouses, workshops, and workrooms!’ ‘How much sickness, death, and misery are produced by the present state of many factories, warehouses, workshops, and workrooms! The places where poor dressmakers, tailors, letter-press printers, and other similar trades have to work for their living, are generally in a worse sanitary condition than any other portion of our worst towns. Many of these places of work were never constructed for such an object. They are badly adapted garrets, sitting-rooms, or bedrooms, generally of an inferior class of house. No attention is paid to cubic space or ventilation. The poor workers are crowded on the floor to a greater extent than occurs with any other kind of over-crowding. The constant breathing of foul air, saturated with moisture, and the action of such air upon the skin renders the inmates peculiarly susceptible of the impression of cold, which is an index indeed of the danger of pulmonary disease to which they are exposed. The result is, that they make bad worse, by over-heating the air and closing up every cranny through which ventilation could be obtained. In such places, and under such circumstances of constrained posture, want of exercise, hurried and insufficient meals, long exhausting labour and foul air – is it wonderful that a great majority of them die early of chest disease, generally of consumption? Intemperance is a common evil of these workshops. The men can only complete their work under the influence of stimulants, which help to undermine their health and destroy their morals, while hurrying them to premature graves. Employers rarely consider these things. Healthy workrooms are no part of the bond into which they enter with their work-people. They pay their money, which they reckon their part of the bargain. And for this wage the workman or workwoman has to give work, health, and life. Do men and women who employ fashionable tailors and milliners ever think of these things? And yet the master is no gainer. His goods are spoiled by foul air and gas fumes, his own health and that of his family suffers, and his work is not so well done as it would be, were his people in health. And the time will come when it will be found cheaper to supply shops, warehouses, and work-rooms with pure air than with foul air.’ ‘And the time will come when it will be found cheaper to supply shops, warehouses, and work-rooms with pure air than with foul air.’ ❂ ✪ C-19: On ‘air-tests’, and measuring CO₂ as a proxy for estimating prevalence of airborne disease indoors ‘Dr. Angus Smith’s air-test, if it could be made of simple application, would be invaluable to use in every sleeping and sick room. Just as without the use of a thermometer no nurse should ever put a patient into a bath, so, if this air-test were made in some equally simple form, should no nurse, or mother, or superintendent, be without it in any ward, nursery, or sleeping-room. But to be used, the air-test must be made as simple a little instrument as the thermometer, and both should be self-registering. ‘...the air-test must be made as simple a little instrument as the thermometer, and both should be self-registering.’ The senses of nurses and mothers become so dulled to foul air that they are perfectly unconscious of what an atmosphere they have let their children, patients, or charges sleep in. But if the tell-tale air-test were to exhibit in the morning, both to nurses and patient and to the superior officer going round, what the atmosphere has been during the night, I question if any greater security could be afforded against a recurrence of the misdemeanour.’ ❂ ✪ C-19: ... And back to the school-room, testing its air, and combatting airborne pathogens ‘And, oh! the crowded national school! where so many children’s epidemics have their origin; and the crowded, unventilated work-room, which sends so many consumptive men and women to the grave; what a tale its air-test would tell! We should have parents saying, and saying rightly, “I will not send my child to that school. I will not trust my son or my daughter in that tailor’s or milliner’s workshop, the air-test stands at ‘Horrid.’” ‘We should have parents saying, and saying rightly, “I will not send my child to that school... the air-test stands at Horrid .”’ And the dormitories of our great boarding schools! Scarlet fever would be no more ascribed to contagion but to its right cause, the air-test standing at “Foul.” We should hear no longer of “mysterious dispensations,” nor of “plague and pestilence” being “in God’s hands,” when, so far as we know, He has put them into our own. The little air-test would both betray the cause of these “mysterious pestilences,” and call upon us to remedy it.’ ❂ ❦ Chapter II – Health of Houses ‘There are five essential points in securing the health of houses:– Pure air. Pure water. Efficient drainage. Cleanliness. Light. Without these, no house can be healthy. And it will be unhealthy just in proportion as they are deficient. To have pure air, your house must be so constructed as that the outer atmosphere shall find its way with ease to every corner of it. ‘To have pure air, your house must be so constructed as that the outer atmosphere shall find its way with ease to every corner of it.’ House architects hardly ever consider this. The object in building a house is to obtain the largest interest for the money, not to save doctor’s bills to the tenants. But, if tenants should ever become so wise as to refuse to occupy unhealthily constructed houses, and if Insurance Companies should ever come to understand their interest so thoroughly as to pay a Sanitary Surveyor to look after the houses where their clients live, speculative architects would speedily be brought to their senses. As it is, they build what pays best. And there are always people foolish enough to take the houses they build. And if in the course of time the families die off, as is so often the case, nobody ever thinks of blaming any but Providence for the result. Ill-informed medical men aid in sustaining the delusion, by laying the blame on “current contagions”. Badly constructed houses do for the healthy what badly constructed hospitals do for the sick.’ ‘Badly constructed houses do for the healthy what badly constructed hospitals do for the sick.’ ❂ ❦ Conclusion ‘The whole of the preceding remarks apply even more to children and to puerperal women than to patients in general. They also apply to the nursing of surgical, quite as much as to that of medical cases. Indeed, if it be possible, cases of external injury require such care even more than sick. In surgical wards, one duty of every nurse certainly is prevention. Fever, or hospital gangrene, or pyæmia, or purulent discharge of some kind may else supervene. If she allows her ward to become filled with the peculiar close fœtid smell, so apt to be produced among surgical cases, especially where there is great suppuration and discharge, she may see a vigorous patient in the prime of life gradually sink and die where, according to all human probability, he ought to have recovered. The surgical nurse must be ever on the watch, ever on her guard, against want of cleanliness, foul air, want of light, and of warmth.’ ‘In surgical wards, one duty of every nurse certainly is prevention.’ ❂ 📖 (Accessed 19 Feb 2024 ~ Original text copied from FiftyWordsForSnow.com) Notes on Nursing (1860) ➤ 📖 (Accessed 19 Feb 2024 ~ Original scanned pages from Google Books) Notes on Nursing (1860) ➤ ❂