➲ Home ➲ C-19 Archives
📖 COVID-19 may put patients at risk for other infections for at least 1 year
‘These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens.’
📖 (2 Apr 2025 ~ CIDRAP) ‘COVID-19 may put patients at risk for other infections for at least 1 year’.
© 2025 S. Soucheray / CIDRAP.
❦ Scientific Media Article ~ ‘COVID-19 may put patients at risk for other infections for at least 1 year’
By Stephanie Soucheray / CIDRAP (2 Apr 2025)
‘In a study yesterday in The Lancet Infectious Diseases, its authors describe how a positive test for COVID-19 is associated with increased rates of diagnosis of various non–SARS-CoV-2 infections in the 12 months following an acute SARS-CoV-2 infection, even if the initial infection is mild to moderate.
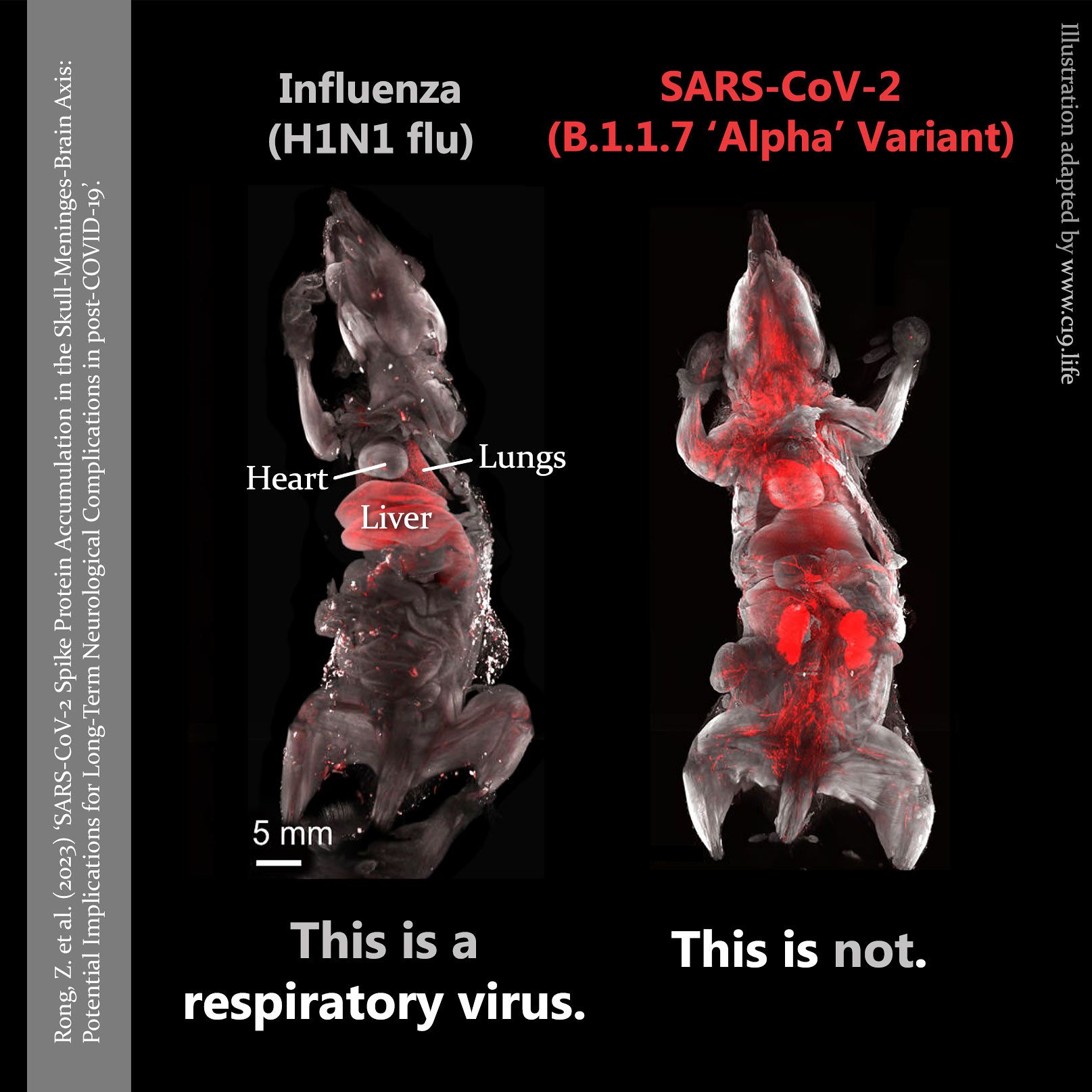
They also found that patients hospitalized for COVID-19 infections were at greater risk for other infections in the year after illness, compared to patients who were hospitalized for influenza.
❦ Almost 50% higher rate of non-COVID respiratory infections
Compared with the test-negative control group, participants with a positive COVID-19 test who were not admitted had significantly increased rates of outpatient diagnosis of bacterial, fungal, and viral infectious illnesses (increased risk of 17%), outpatient respiratory infections (increased risk of 46%), and admission to hospital for infectious illnesses (increased risk of 41%), including for sepsis and respiratory infections.
Overall, non-hospitalized COVID patients had higher rates in 32% of the 65 laboratory-based outcomes compared to those who tested negative for SARS-CoV-2.
That rate jumped in hospitalized COVID-19 patients, who had higher rates of positive results in 71% of the examined laboratory tests, after accounting for multiple comparisons with the COVID-negative cohort.
❦ COVID may alter immune function
To further analyze the association between COVID-19 and subsequent infections, the authors compared people admitted to the hospital for seasonal influenza (3,293) and those admitted for COVID-19 (12,450) in the VA database, and found that COVID patients had higher rates of admission to hospital for infectious illnesses (increased risk of 24%), admission to hospital for sepsis (increased risk of 35%), and in-hospital use of antimicrobials (increased risk of 23%).
“These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens,” Chodick writes in a Lancet Comment on the study.
“The evidence suggests effects extending beyond the acute phase of infection, affecting even mild cases.”’
❂
📖 (2 Apr 2025 ~ CIDRAP) COVID-19 may put patients at risk for other infections for at least 1 year ➤
© 2025
Stephanie Soucheray
/
CIDRAP.
❂
📖 (1 Apr 2025 ~ The Lancet: Infectious Diseases) ‘Rates of infection with other pathogens after a positive COVID-19 test versus a negative test in US veterans (November 2021 to December 2023): a retrospective cohort study’.
© 2025 Cai et al / The Lancet: Infectious Diseases.
❦ Study ~ ‘Rates of infection with other pathogens after a positive COVID-19 test versus a negative test in US veterans (November 2021 to December 2023): a retrospective cohort study’
By Cai et al / The Lancet: Infectious Diseases (1 Apr 2025)
‘In the 12 months of follow-up, compared with participants who had a negative test for COVID-19, people with COVID-19 who did not require admission to hospital during the acute phase of infection had increased test positivity rates for bacterial infections (in blood, urine, and respiratory cultures) and viral diseases (including Epstein–Barr virus, herpes simplex virus reactivation, and respiratory viral infections).
People who were positive for COVID-19 and admitted to hospital also had increased rates of bacterial infections in blood, respiratory, and urine biospecimens, and viral infections in blood and respiratory biospecimens.
Analyses of pre-specified outcomes showed that, compared with the test-negative control group, participants with a positive COVID-19 test who were not admitted to hospital had significantly increased rates of outpatient diagnosis of infectious illnesses (increased risk of 17%), including bacterial, fungal, and viral infections; outpatient respiratory infections (increased risk of 46%); and admission to hospital for infectious illnesses (increased risk of 41%), including for sepsis and respiratory infections; the rates of pre-specified outcomes were generally higher among those who were admitted to hospital for COVID-19 during the acute phase.
❦ COVID-19 vs. seasonal influenza
Compared with people admitted to hospital for seasonal influenza, those admitted for COVID-19 had higher rates of admission to hospital for infectious illnesses (increased risk of 24%), admission to hospital for sepsis (increased risk of 35%), and in-hospital use of antimicrobials (increased risk of 23%).’
❂
📖 (1 Apr 2025 ~ The Lancet: Infectious Diseases) Rates of infection with other pathogens after a positive COVID-19 test versus a negative test in US veterans (November 2021 to December 2023): a retrospective cohort study ➤
© 2025
Cai
et al
/
The Lancet: Infectious Diseases.
❂
📖 (1 Apr 2025 ~ The Lancet: Infectious Diseases ~ Comment) ‘Long-term infectious sequelae after SARS-CoV-2 infection should be considered in mild cases too’.
© 2025 Gabriel Chodick / The Lancet: Infectious Diseases ~ Comment.
❦ Comment ~ ‘Long-term infectious sequelae after SARS-CoV-2 infection should be considered in mild cases too’
By Gabriel Chodick / The Lancet: Infectious Diseases ~ Comment (1 Apr 2025)
❦ ‘Cai and colleagues contribute important insights into a previously under-explored consequence: the elevated rates of subsequent infections following SARS-CoV-2 infection, including in people who had not been admitted to hospital for COVID-19 or developed post-COVID-19-condition (also known as long COVID).
To establish whether these increased infection rates were unique to SARS-CoV-2, Cai and colleagues conducted comparative analyses with patients who were admitted to hospital for influenza.
Patients admitted to hospital for COVID-19 showed higher rates of all-cause admissions to hospital and infectious illness-related hospitalisations, including sepsis and positive urine and blood cultures, compared with patients admitted to hospital for influenza.
These findings complement a previous VA cohort study from the same group, which showed 51% greater all-cause mortality hazard in the COVID-19 group versus the influenza group.
A key advancement of Cai and colleagues’ study is the identification of increased infection rates among patients who were not admitted to hospital [for COVID-19].
‘While previous research has primarily shown elevated rates of infection in patients with long-COVID, or in those requiring admission to hospital, this analysis demonstrates substantial increases in infection rates even in those with mild initial disease.’
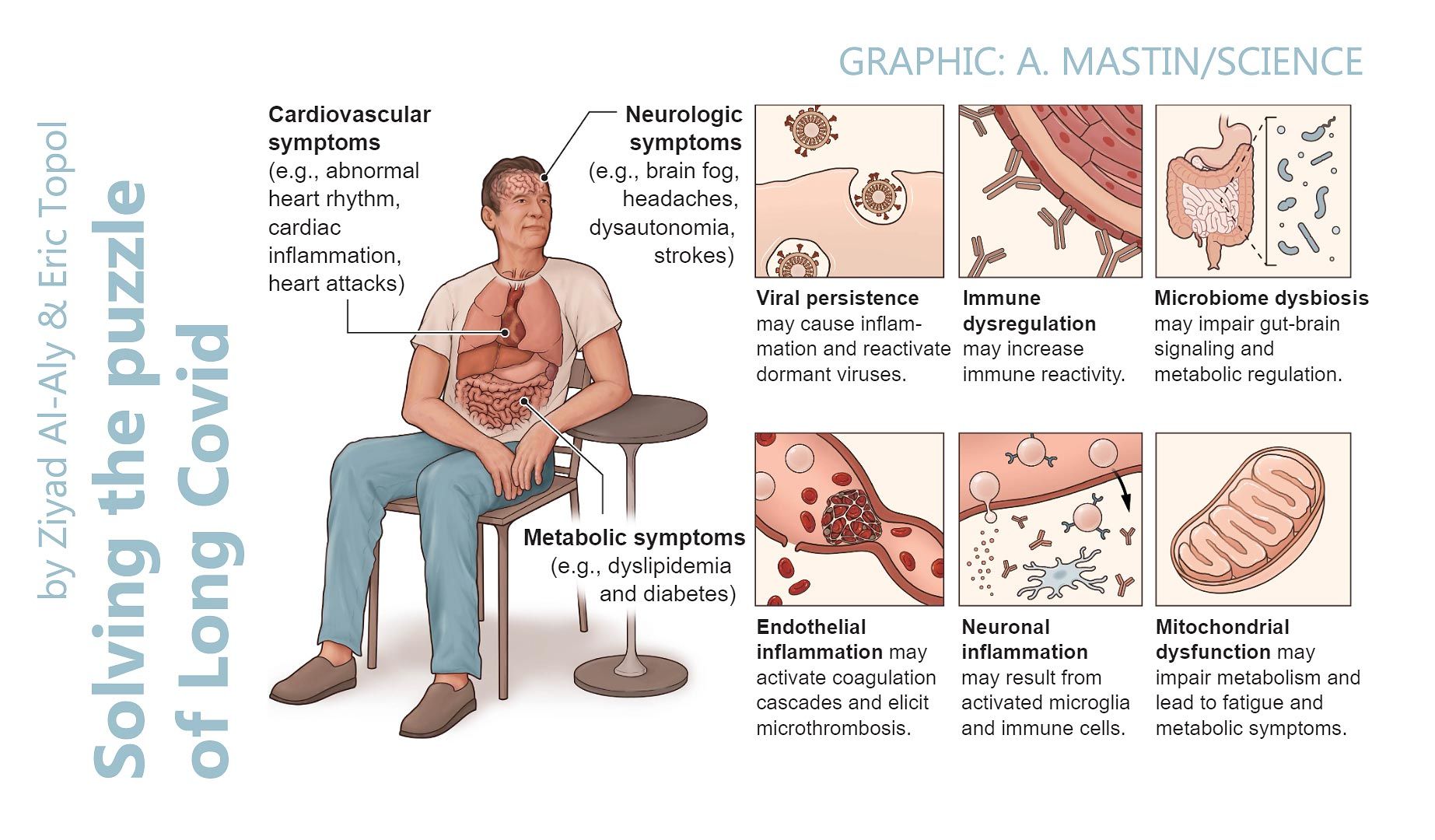
This builds upon another analysis of VA healthcare data, which showed increased rates of various non-communicable conditions in patients with COVID-19 who were not admitted to hospital, including pulmonary diseases, hyperglycemia, diabetes, kidney disease, and gastrointestinal complications.
‘These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens.
‘The evidence suggests effects extending beyond the acute phase of infection, affecting even mild cases.’
This growing body of research on post-acute COVID-19 sequelae supports a bi-directional relationship between non-communicable diseases and infectious diseases, resulting in persistently increased risk of adverse outcomes in the months and years after initial SARS-CoV-2 infection.’
❂
📖 (1 Apr 2025 ~ The Lancet: Infectious Diseases ~ Comment) Long-term infectious sequelae after SARS-CoV-2 infection should be considered in mild cases too ➤
© 2025
Gabriel Chodick
/
The Lancet: Infectious Diseases ~ Comment.
❂
More... Immunity
More... PASC (‘Long COVID’)
C-19: Archives
Useful search tags:
air filtration / babies & children / body / brain / C19.Life / cancer / comment / dementia / economy / elders / excess deaths / exercise / flu / heart / history / hospitals / immunity / influenza / law / Lisa Iannattone / long covid / lungs / mitochondria / muscles / musculoskeletal / NHS / Noor Bari / nosocomial / PEM / parkinson’s / propaganda / reinfections / reproduction and pregnancy / resources / respirators / respiratory / risk / SARS(-CoV-1) / schools / solutions / transmission / universities / UVC / vaccines / variants / WHO / young adults / zoonosis