➲ Home ➲ C-19 Archives
📖 Does COVID increase the risk of Alzheimer’s disease?
‘Scientists discover that even mild COVID-19 can alter brain proteins linked to Alzheimer’s disease, potentially increasing dementia risk.
COVID-19-positive individuals exhibited lower cognitive test performance compared to controls – equivalent to almost two years of age-related cognitive decline.’
📖 (2 Feb 2025 ~ News Medical Life Sciences) ‘Does COVID increase the risk of Alzheimer’s disease?’
© 2025 Dr. Chinta Sidharthan / News Medical Life Sciences.
‘Participants who had mild or asymptomatic COVID-19 showed alterations in their plasma biomarkers, suggesting that the infection’s impact on brain health may not be limited to severe cases.’
❦ Scientific Media Article ~ ‘Does COVID increase the risk of Alzheimer’s disease?’
By Dr. Chinta Sidharthan / News Medical Life Sciences (2 Feb 2025)
‘A recent study published in the journal Nature Medicine investigated whether both mild and severe cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection are linked to changes in brain biomarkers associated with Alzheimer’s disease.
By analyzing blood samples from the United Kingdom (U.K.) Biobank participants, the researchers found that individuals who had COVID-19 showed signs of increased brain pathology, raising critical public health concerns.
Alzheimer’s disease is associated with changes in brain proteins such as beta-amyloid and tau, which can be detected in blood samples years before disease symptoms appear.
However, previous studies have focused mainly on severe COVID-19 cases, leaving a gap in understanding the risks for those with mild-to-moderate infections.
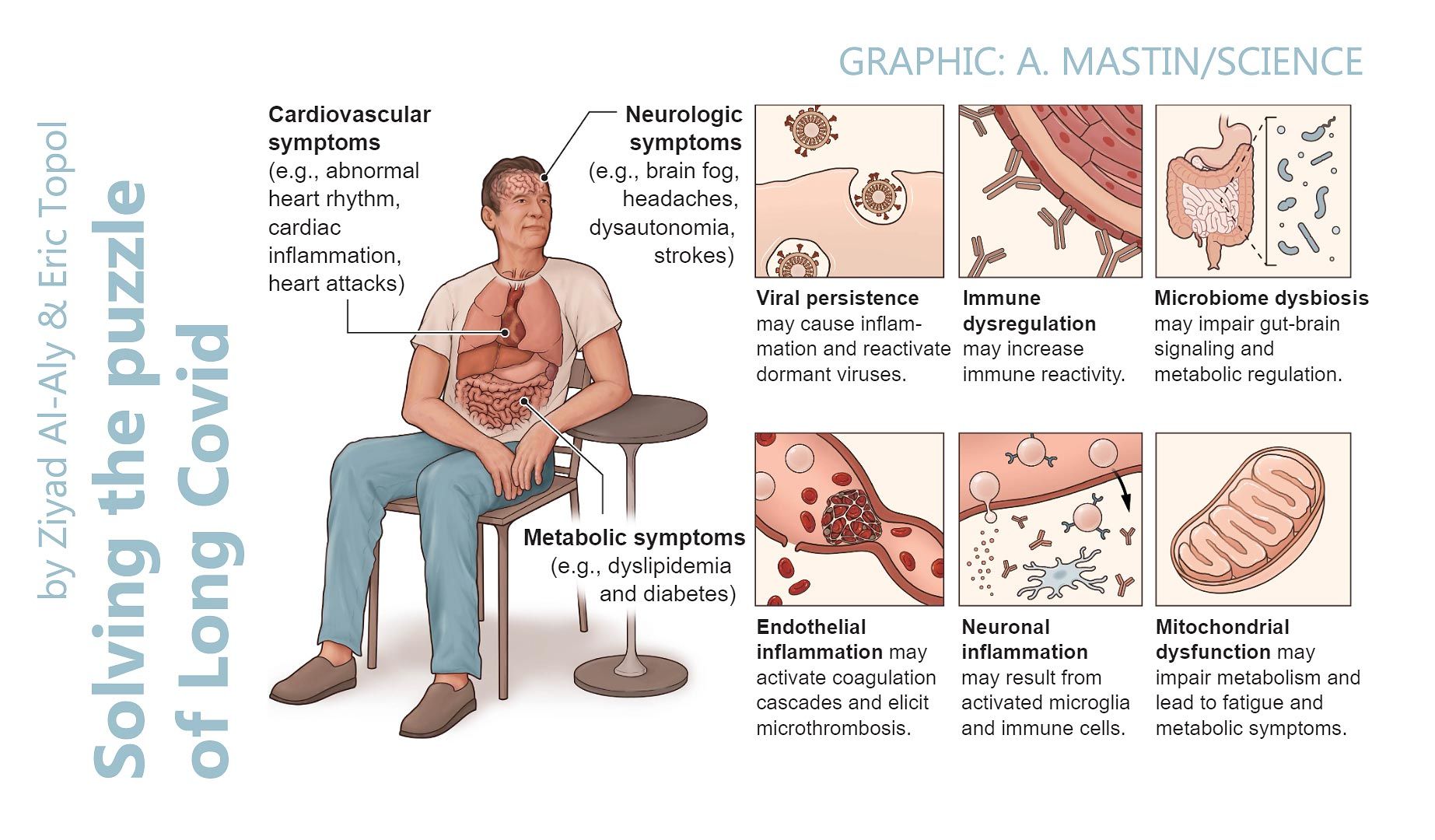
Given the emerging evidence that even mild or moderate cases of COVID-19 can result in Post-Acute Sequelae of COVID-19 (PASC), this study aimed to determine whether SARS-CoV-2 infection – regardless of severity – could contribute to changes in these critical biomarkers.
‘The study found that individuals who had COVID-19 exhibited significant changes in brain biomarkers associated with Alzheimer’s disease.’
The Aβ42:Aβ40 ratio, a key marker of beta-amyloid build-up, was lower in COVID-19-positive participants compared to their matched controls. A reduced ratio of these proteins is commonly linked to Alzheimer’s pathology.
Additionally, the study observed increased levels of pTau-181, a protein associated with tau tangles in the brain, and elevated NfL levels, which indicated neuronal damage. GFAP, a marker of astrocyte activation and neuroinflammation, was also higher in those who had COVID-19.
‘Strikingly, these biomarker changes were comparable to four years of aging or 60% of the effect size of inheriting a single APOE-ε4 allele, a well-known genetic risk factor for Alzheimer’s disease.’
These biomarker changes were more pronounced in older individuals (particularly those over 70 years old) and those with pre-existing risk factors such as hypertension and obesity.
‘Interestingly, even participants who had mild or asymptomatic COVID-19 showed alterations in their plasma biomarkers, suggesting that the infection’s impact on brain health may not be limited to severe cases.
The researchers also analyzed cognitive test scores and neuroimaging data, finding that COVID-19-positive individuals exhibited lower cognitive test performance compared to controls – equivalent to almost two years of age-related cognitive decline.’
Brain imaging revealed structural patterns associated with Alzheimer’s disease in some participants, further reinforcing the potential link between COVID-19 and neurodegeneration.
Additionally, the study found that certain inflammatory markers, including TNFSF10 (TRAIL), PTX3, and IL-6, were altered in post-COVID individuals, suggesting a prolonged inflammatory response that could contribute to brain pathology.
The researchers explained that while this study does not establish a direct causal link between COVID-19 and Alzheimer’s, the results raise concerns about the potential long-term neurological consequences of the viral infection.
The findings also highlighted the importance of monitoring brain health in post-COVID-19 patients and considering preventive strategies for at-risk patients.
‘Overall, the study provided new evidence that COVID-19 may accelerate Alzheimer’s disease-related brain changes, even in individuals with mild infections.’
The observed alterations in plasma biomarkers suggested a potential long-term impact on brain health.
‘While further research is needed to confirm these findings, the authors emphasized that their results align with previous reports suggesting an increased incidence of dementia following COVID-19.’
These findings highlight the importance of long-term monitoring, preventive interventions, and future public health strategies aimed at mitigating post-COVID neurological risks.’
📖 (2 Feb 2025 ~ News Medical Life Sciences) ‘Does COVID increase the risk of Alzheimer’s disease’
© 2025 Dr. Chinta Sidharthan / News Medical Life Sciences.

📖 (2 Feb 2025 ~ News Medical Life Sciences) Does COVID increase the risk of Alzheimer’s disease? ➤
© 2025 Dr. Chinta Sidharthan / News Medical Life Sciences.
❂
📖 (30 Jan 2025 ~ Nature Medicine) ‘Plasma proteomic evidence for increased β-amyloid pathology after SARS-CoV-2 infection’.
© 2025 Duff et al / Nature Medicine.
❦ Study ~ ‘Plasma proteomic evidence for increased β-amyloid pathology after SARS-CoV-2 infection’
By Duff et al / Nature Medicine (30 Jan 2025)
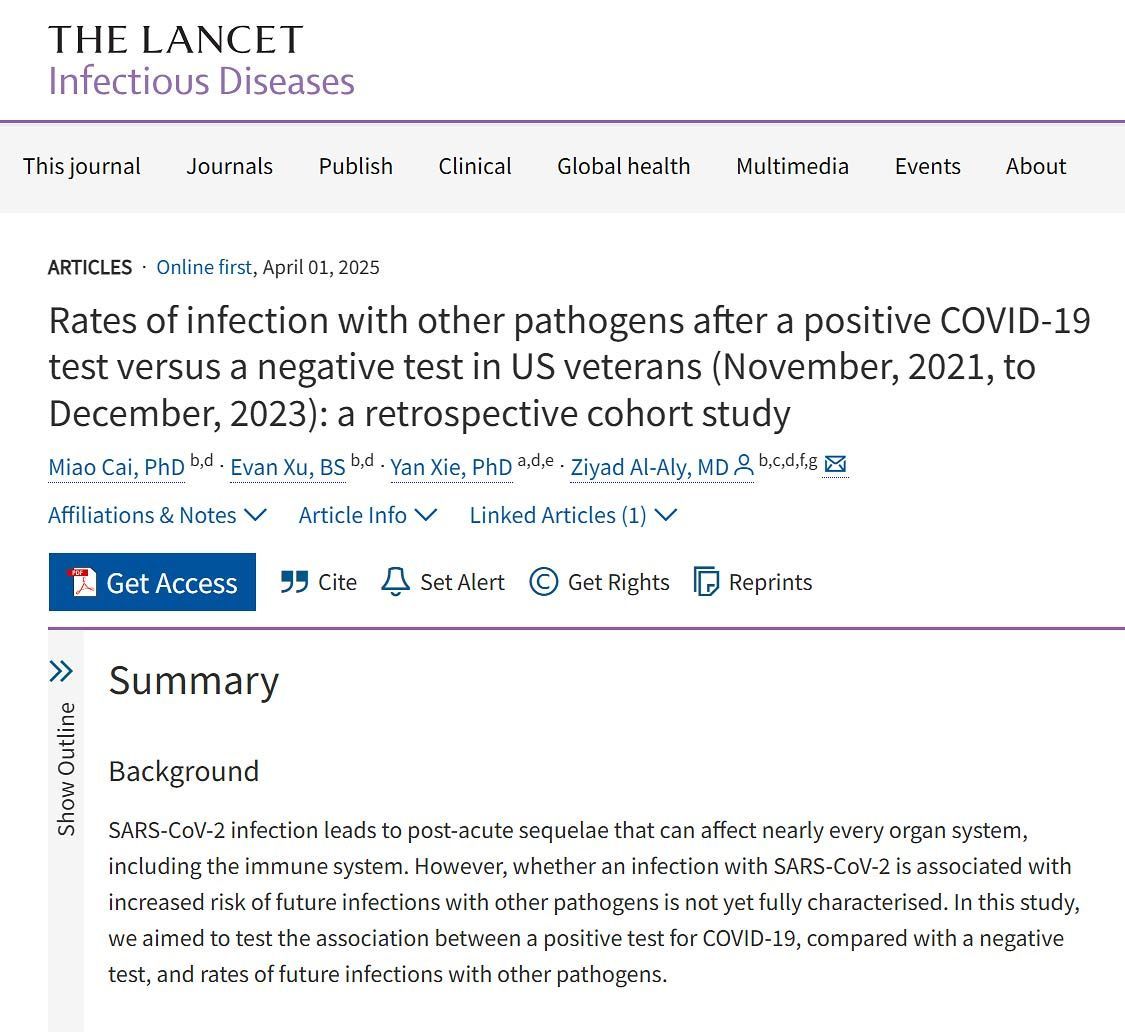
‘In conclusion, our study found plasma biomarker changes related to higher brain β-amyloid pathology in association with enhanced brain imaging signatures of Alzheimer’s Disease (AD) after SARS-CoV-2 infection.
While the study does not establish a causal link between infection and AD, along with earlier studies suggesting increased rates of dementia diagnosis following COVID-19, it suggests that the incidence of AD could increase following the COVID-19 pandemic.
Importantly, the relationships described here may not be specific for SARS-CoV-2 and reflect more general effects of infections on the aging brain.
Prevention of SARS-CoV-2 infection (and other systemic infections) therefore should be considered in developing risk factor modification strategies for AD in later life.’
📖
(30 Jan 2025 ~ Nature Medicine) Plasma proteomic evidence for increased β-amyloid pathology after SARS-CoV-2 infection
➤
© 2025 Duff et al / Nature Medicine.
❂
❦ Related reading
📖 (15 Dec 2024 ~ BMC Geriatrics) Association between COVID-19 infection and new-onset dementia in older adults: a systematic review and meta-analysis ➤
© 2024 Shan et al / BMC Geriatrics.
📖 (3 Dec 2024 ~ eNeurologicalSci) Impact of COVID-19 on functional, cognitive, neuropsychiatric, and health-related outcomes in patients with dementia: A systematic review ➤
© 2024 Crivelli et al / eNeurologicalSci.
📖 (3 Mar 2025 ~ Age Ageing) Risk of new-onset dementia following COVID-19 infection: a systematic review and meta-analysis ➤
© 2025 Zhang et al / Age Ageing.
📖 (29 Jun 2023 ~ Nature Cell Death Discovery: Review Article) Long-term effects of SARS-CoV-2 infection on human brain and memory ➤
© 2023 Ding & HanJun / Nature Cell Death Discovery.
📖 (Nov 2024 ~ The Lancet) Temporal association between COVID-19 infection and subsequent new-onset dementia in older adults (aged 60 years and above): a systematic review and meta-analysis ➤
© 2024 Shan et al / The Lancet.
📖 (7 Dec 2021 ~ Alzheimer’s & Dementia Journal) Impact of COVID-19 on the Onset and Progression of Alzheimer’s Disease and Related Dementias: A Roadmap for Future Research ➤
© 2021 Gordon et al / Alzheimer’s & Dementia Journal.
More... Dementia
More... Brain & Nervous System
C-19: Archives
Useful search tags:
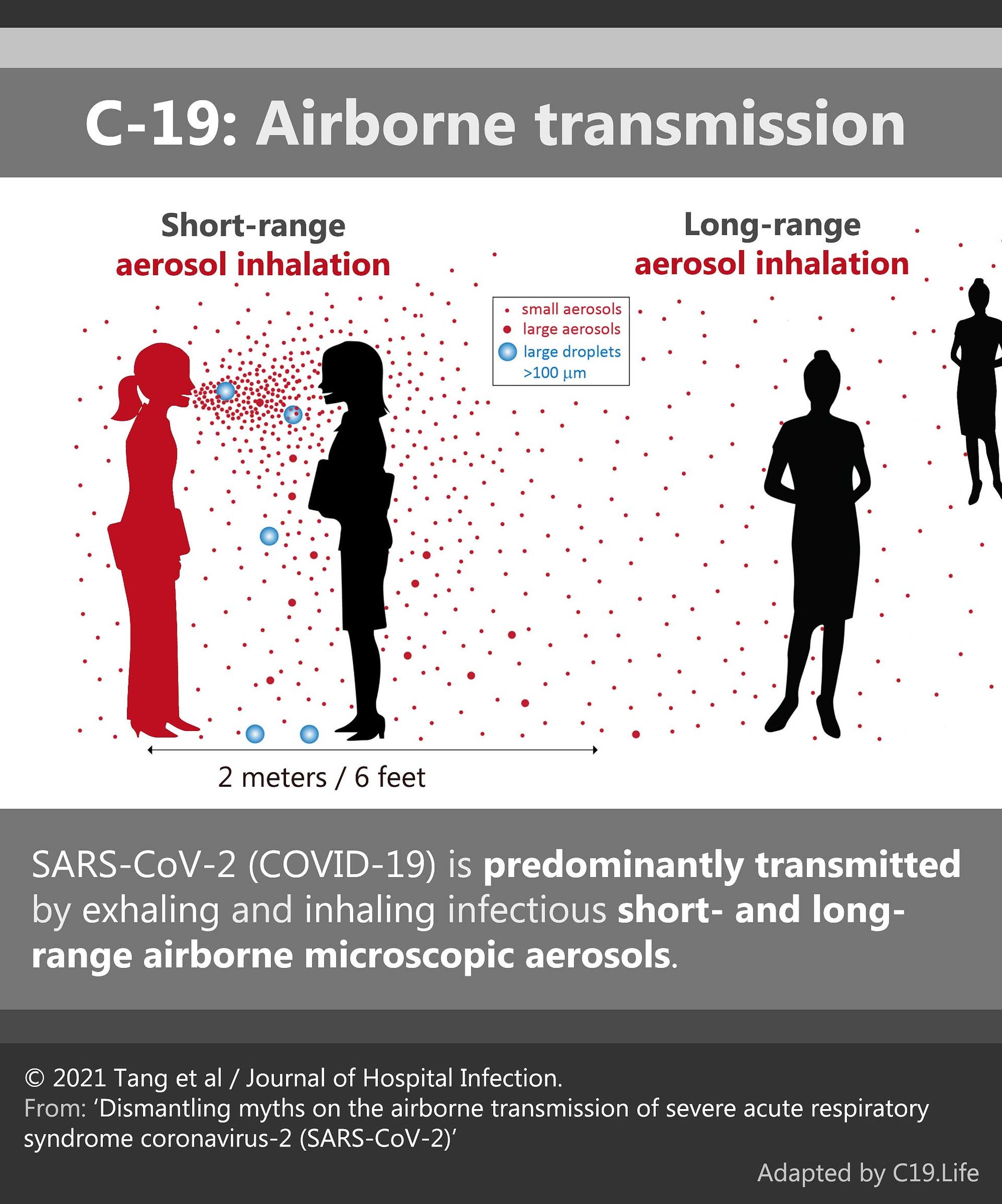
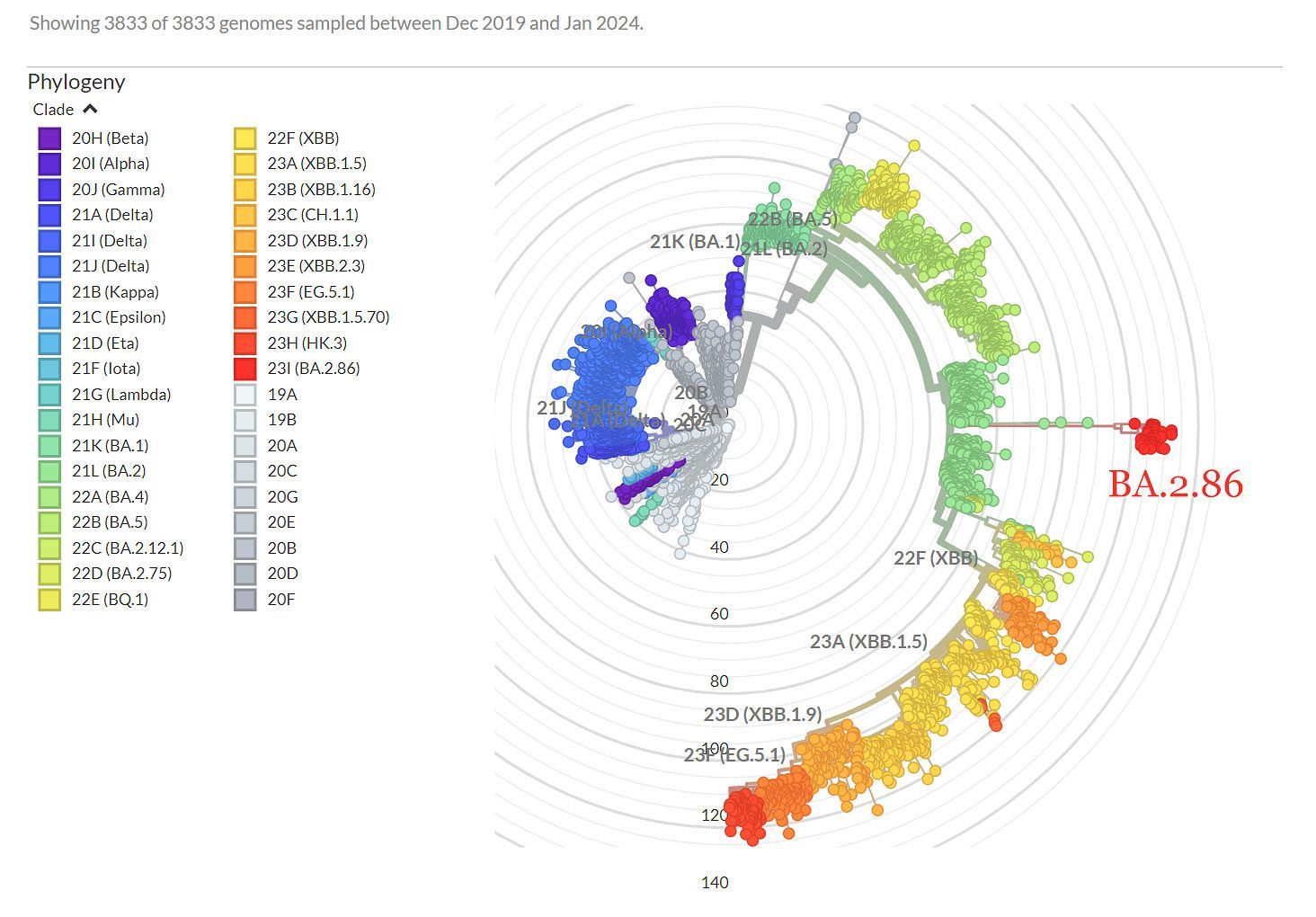
air filtration / babies & children / body / brain / C19.Life / cancer / comment / dementia / economy / elders / excess deaths / exercise / flu / heart / history / hospitals / immunity / influenza / law / Lisa Iannattone / long covid / lungs / mitochondria / muscles / musculoskeletal / NHS / Noor Bari / nosocomial / PEM / parkinson’s / propaganda / reinfections / reproduction and pregnancy / resources / respirators / respiratory / risk / SARS(-CoV-1) / schools / solutions / transmission / universities / UVC / vaccines / variants / WHO / young adults / zoonosis