➲ Home ➲ C-19 Archives
On science, common sense, and keeping healthcare-acquired infections (HAIs) at bay
❦ I keep saying that someday I’ll write a book about the struggle to bring an engineering perspective to infection prevention and control in healthcare.
For now... just an essay.
Is there anything worse than knowing that there are oceans full of icebergs ahead; how easy it is to engineer systems to detect and steer around them; but not being able to get the owners of the liners (or anyone in command) to listen as you blindly head straight for them?
I’ve been advocating for engineering solutions and standards for air, water and surfaces in healthcare facilities to lower disease transmission for over 30 years.
The irony of being accused by out-of-touch ID/PH/IPAC/Epi* of epistemic trespassing before and during the pandemic is gobsmacking.
* ID = Infectious Diseases / PH = Public Health / IPAC = Infection Prevention and Control / Epi = Epidemiology.
I started with single patient rooms.
In pre-pandemic Canada, we had the highest HAI* rate in OECD* – one in ten inpatients – and the lowest beds and lowest single rooms per capita.
* HAI = Hospital-Acquired Infection, also known as a nosocomial infection, is an infection that patients get in healthcare facilities while receiving treatment for other medical or surgical conditions.
* OECD = Organisation for Economic Co-operation and Development.
We also had sicker patients.
Studies now show that single-patient rooms cut infection rates in half.
Ten years ago, Canada began moving to primarily single-patient rooms for new hospital builds – although not a hundred percent as hospitals won’t give up preferential private-room billing to insurance companies.
In 2007, we formed a small group of volunteers to create a Canadian National Standard for Plume Evacuation – source control to prevent airborne transmission of disease in ORs*.
* OR = Operating Room.
Despite nurses’ complaints, we couldn’t get support – until doctors started getting genital warts in their noses.
We helped ISO* develop a similar global standard which was published in 2014.
* ISO = International Organization for Standardization.
Because laser and electrocautery smoke is clearly visible, and there are now national and international standards, the practice of source control in ORs is now well-accepted.
Unlike smoke, our breath is not visible – and there are no national or international standards yet for pathogen-free air.
However, the principle of air extraction would work in ICUs* and patient rooms just as well as ORs.
* ICU = Intensive Care Unit.
Copper was registered as an antimicrobial in 2008, 50 years after silver.
Over the past ten years, countless studies have shown efficacy, persistence, durability and the safety of copper surfaces – but the ID community pushes back with objective conclusions like “... Too good to be true”.
While ID/IPAC has no budget of their own to implement engineering measures in hospitals, in Canada they can (and most often do) scuttle initiatives in Engineering and Facilities Management, and in Environmental Services departments, to introduce new technologies and materials to combat HAIs.
In 2011, I pursued the concept of combining continuous and high-frequency bioburden reduction of surfaces to prevent fomite transmission.
Copper could provide ‘continuous’ reduction on high-touch surfaces, while UV* (if automated) could provide ‘high-frequency’ reduction on all surfaces.
* UV = Ultraviolet (UV) radiation.
In 2014 we launched AutoUV – built-in fixtures that detected occupancy, monitored whether doors were open or closed, and dosed rooms every four hours and after every exit.
As expected, it works.
It can’t not work.
And after seven years in the field, it’s been shown to be extremely safe.
Bathrooms can be the source of half of disease spread in hospitals.
C diff* can be colonized in air after every toilet flush. Aerosols drift for minutes to hours. Intestinal and respiratory diseases are often spread through toilet aerosolization.
* C. diff, also known as Clostridioides difficile or C. difficile, is a gram-positive bacterium that can cause diarrhoea and colitis.
AutoUV? Bathroom source-control.
Today, there are thousands of units in use across Canada – and the Ontario Ministry of Health has made AutoUV a standard-of-care for new hospital builds.
MOHLTC* now mandates and funds AutoUV.
* MOHLTC = Ontario Ministry of Health and Long Term Care.
Hooray.
But IPAC stubbornly pushes back against the use of AutoUV.
In other ironic news, Health Canada is cutting off use of open-air UV in healthcare, including Upper Air UV – in the middle of an airborne pandemic – due to a flood of household UV devices that are being sold retail and online that don’t work, don’t have safety certificates, or produce [dangerous] ozone.
In 2014 I co-founded CHAIR – the Coalition for Healthcare-Acquired Infection Reduction – a group of scientists, engineers, ID doctors and industry partners working together to engineer air, water and surfaces in order to lower HAIs.
We naively thought that we could achieve an 80 percent decrease in preventable, environmental HAIs with new technologies and materials.
We knew legacy industry players in chemical disinfection would be a challenge.
We had no idea that the biggest battle would come from the ID/IPAC community itself.
I watched in horror at the denial of airborne transmission of 2003 SARS at a plenary session in Toronto in May 2014.
Playing to the crowd in a purposeful, dismissive and comedic way, the speaker claimed that “SARS is not airborne. The droplets fall to the floor within six feet.”
Dr Yu, of Hong Kong Public Health, had only just re-analyzed and re-published the Amoy Gardens study six months earlier on the 10-year anniversary reaffirming airborne transmission of [the original 2002-2004] SARS.
When I challenged the speaker, he exclaimed:
— “Oh, don’t worry. I know him. He's changed his mind.”
In 2014, an ID doc from PHO* presented at a Toronto IPAC Education Day.
* PHO = Public Health Ontario.
He claimed that Ebola was definitely not airborne. When challenged with a study showing transmission between caged and separated laboratory primates, he replied:
— “Well, monkeys have long arms. Besides, they can spit.”
In a follow-up from me: “There’s airborne transmission of PRRV* in hogs between factory farms kilometers away, and documented in Veterinary journals...”
* PRRV = Porcine reproductive and respiratory syndrome virus.
— “I don’t read those journals.”
— “Would you like me to send you some articles?”
— “Don’t bother.”
They don’t want to know.
Hospitals are a global network of MDRO* incubators.
* MDRO = A multidrug-resistant organism (MDRO) is a germ that is resistant to multiple types of antibiotics, making it difficult to treat and cure infections.
CDI* and MRSA* initially tend to spread in hospitals before seeding community-acquired versions. Sinks and drains are known sources of contamination, especially via the aerosol route. Pathogens are getting more virulent – including MDRO/CPE/CRE/CPOs and C auris.
* CDI = Clostridioides difficile infection (CDI or C-diff), also known as Clostridium difficile infection, is a symptomatic infection due to the spore-forming bacterium Clostridioides difficile.
* MRSA = Methicillin-resistant Staphylococcus aureus (MRSA) infection is caused by a type of staph bacteria that's become resistant to many of the antibiotics used to treat ordinary staph infections.
Water contamination and aerosolization, and bacterial, fungal and biofilm reservoir control = Engineering.
Progressive examples:
➲ In Calgary Health Region: UV all incoming water? No Legionella. Self-disinfecting sinks? Electrocatalytically-split H2O into OH-, O-, O3 and H2OH = Disinfectant.
➲ In Ontario, the Ministry of Health now funds and mandates self-disinfecting sink and drain technologies.
However, IPAC/ID continue to push back against new technologies.
So why write this essay?
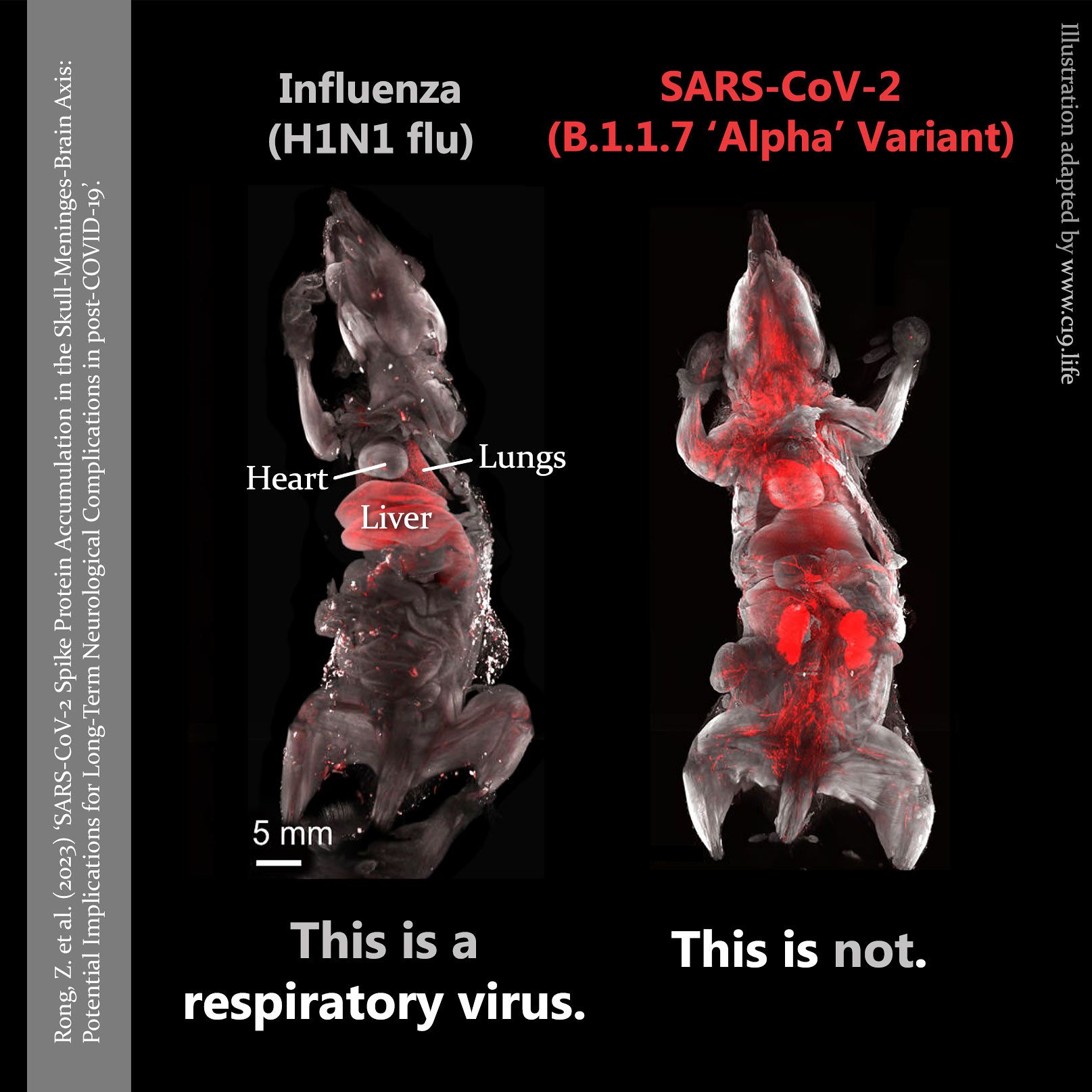
Because the current struggle to recognize airborne transmission, and the engineered solutions, is part of an epic struggle.
We’ve seen how much resistance there has been in almost two years.
The entrenchment started a century ago, as most of us know. But the struggle has been about much more than “airborne”.
It’s a struggle for epistemic control; for critical thinking; for evaluation to first principles; the applied use of deductive reasoning; politics; economics; tension between careerism, and the Precautionary Principle.
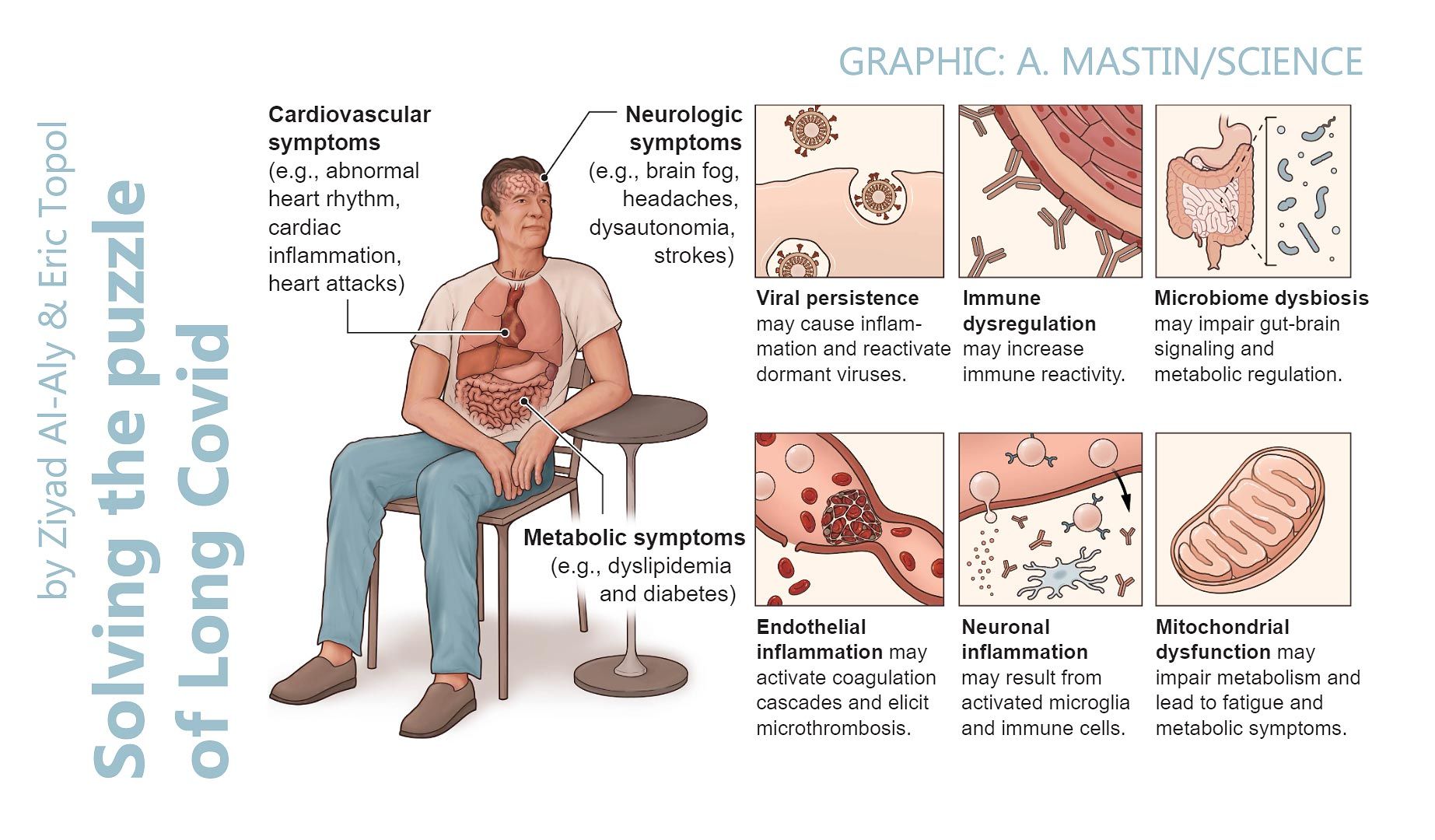
Many in ID/PH have fought against engineering measures, but now are giving up on fighting the virus at all. It’s important to not give into the temptation of accepting that “We just have to live with it,” or that “It’s endemic now” – or “It's mild”.
No. Not acceptable.
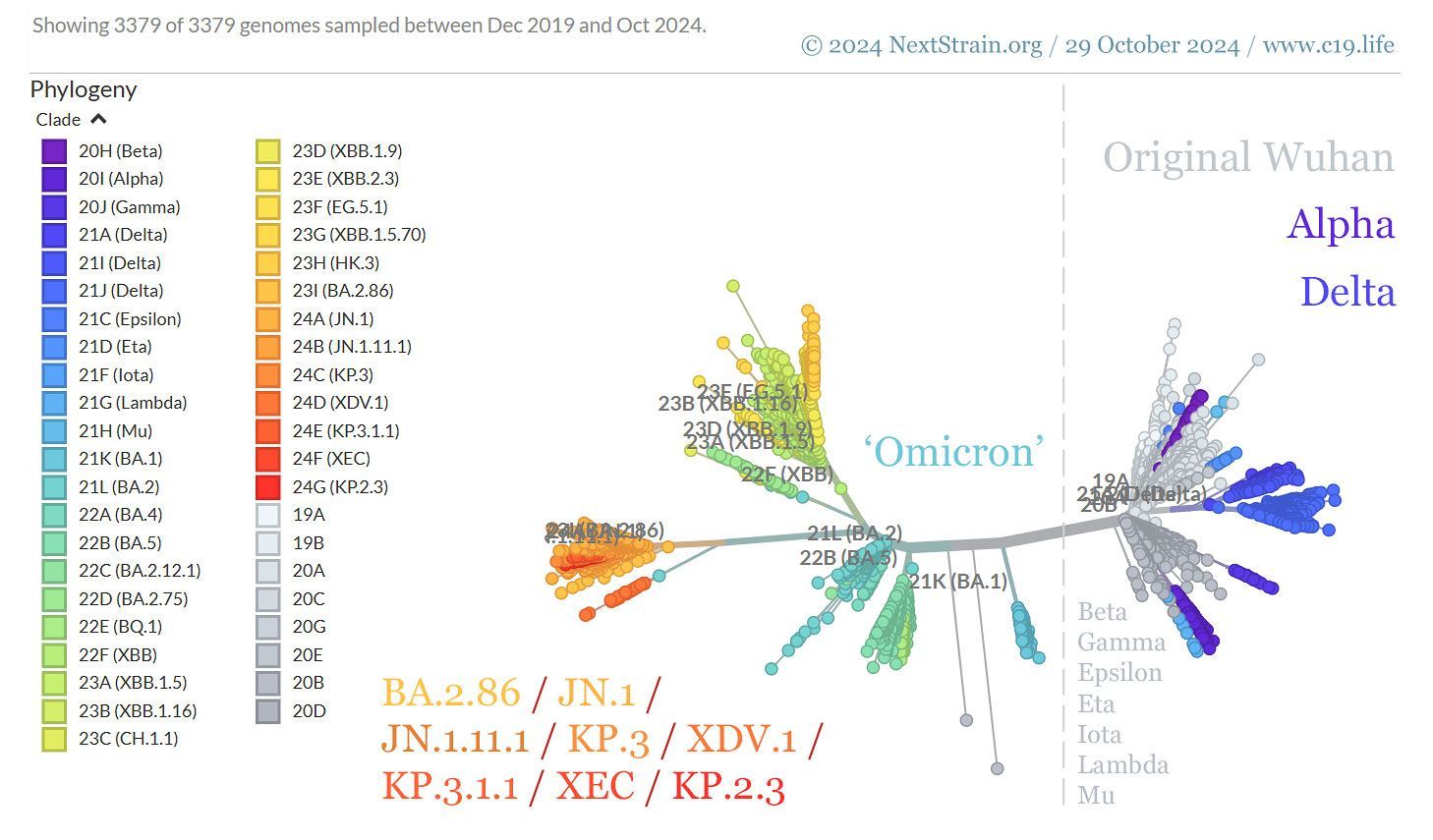
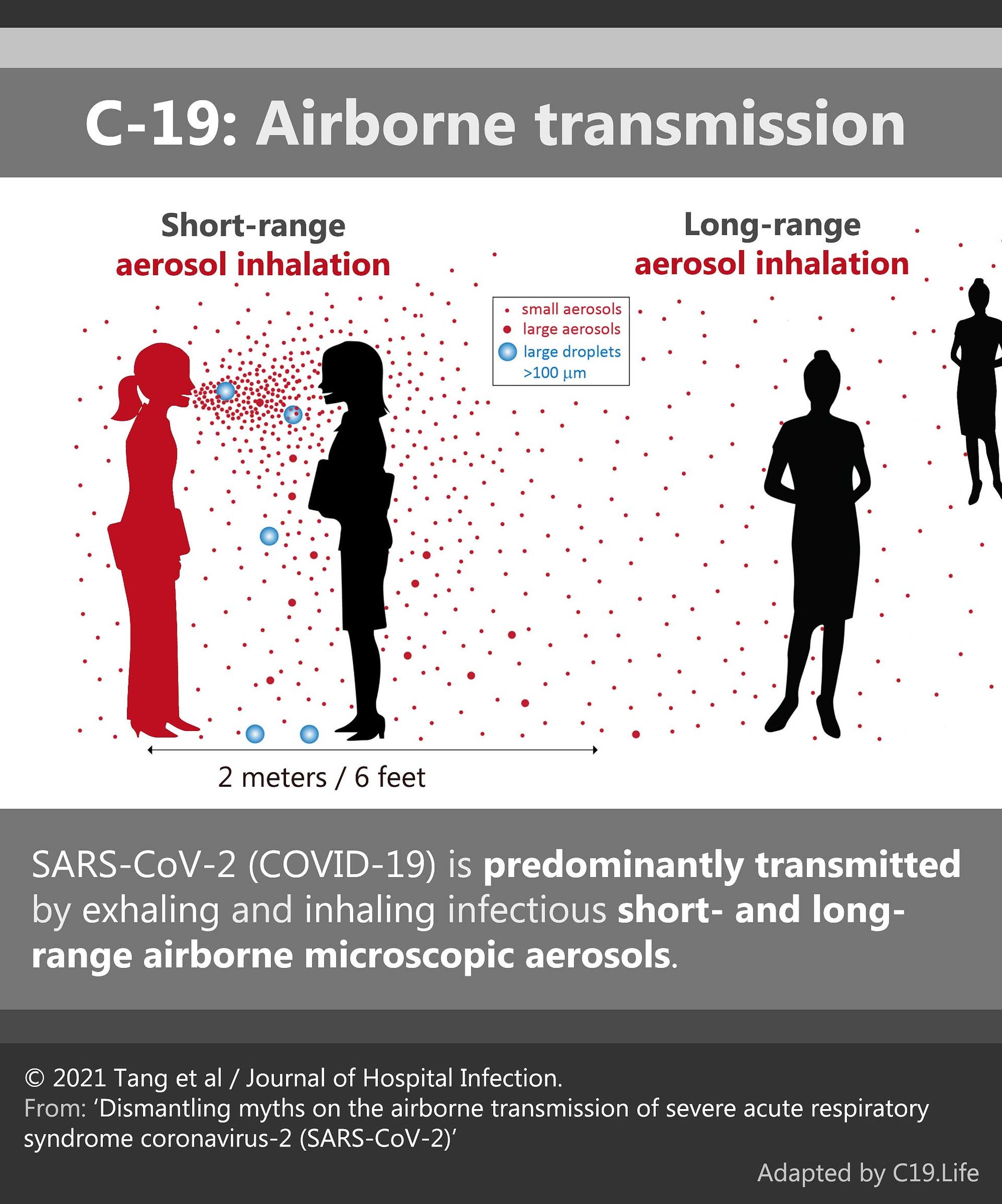
COVID-19 is airborne. It’s very manageable.
Wear an N95 [FFP2 respirator] in occupied spaces until case counts are near zero. Make indoor air safe – ventilate, filter it, and use UV.
Set national and international standards for safe indoor air.
Set a goal of elimination – first regional, then national, and then global.
❂
© 2021
Barry Hunt.
➲
C-19: Archives
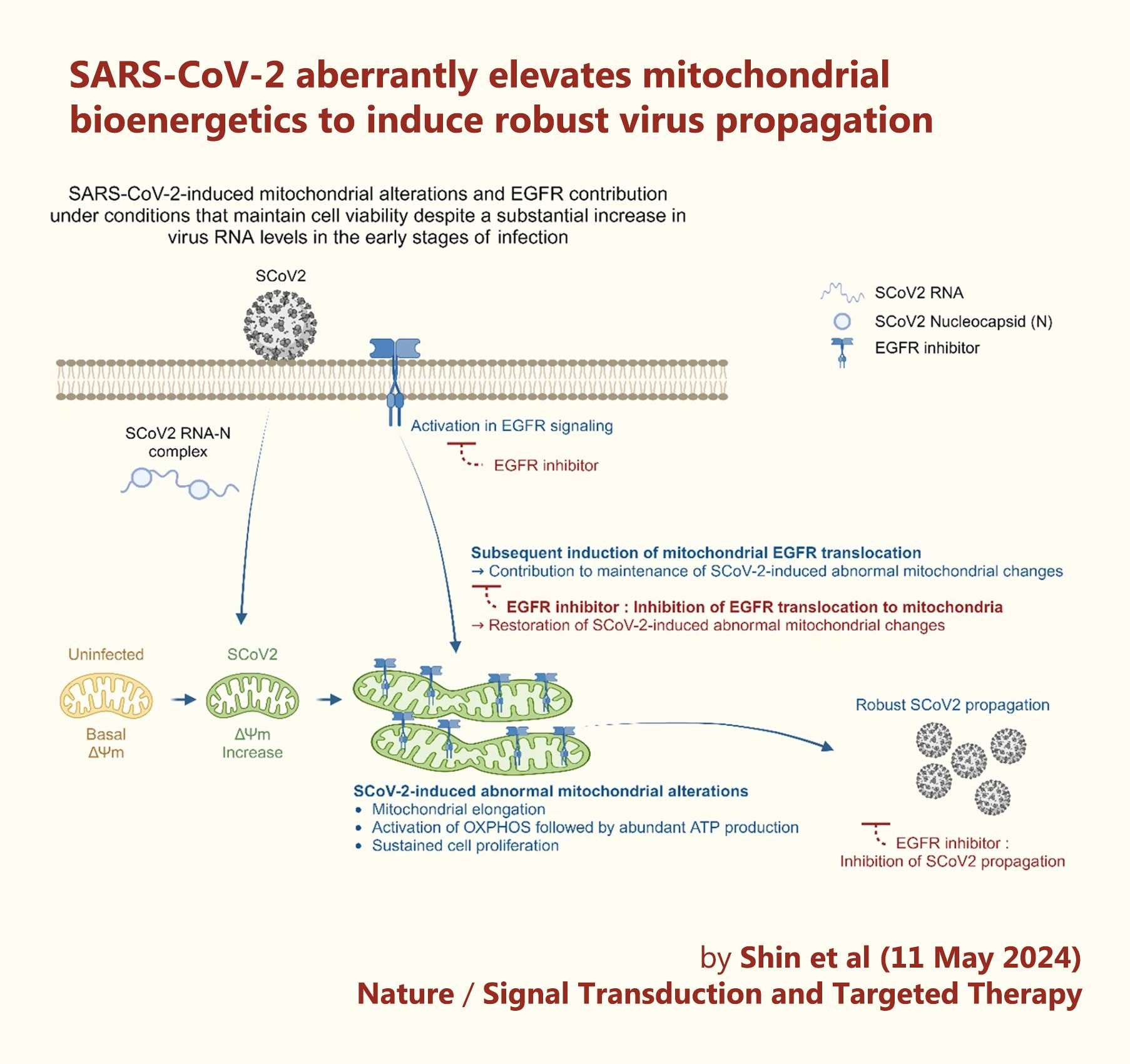
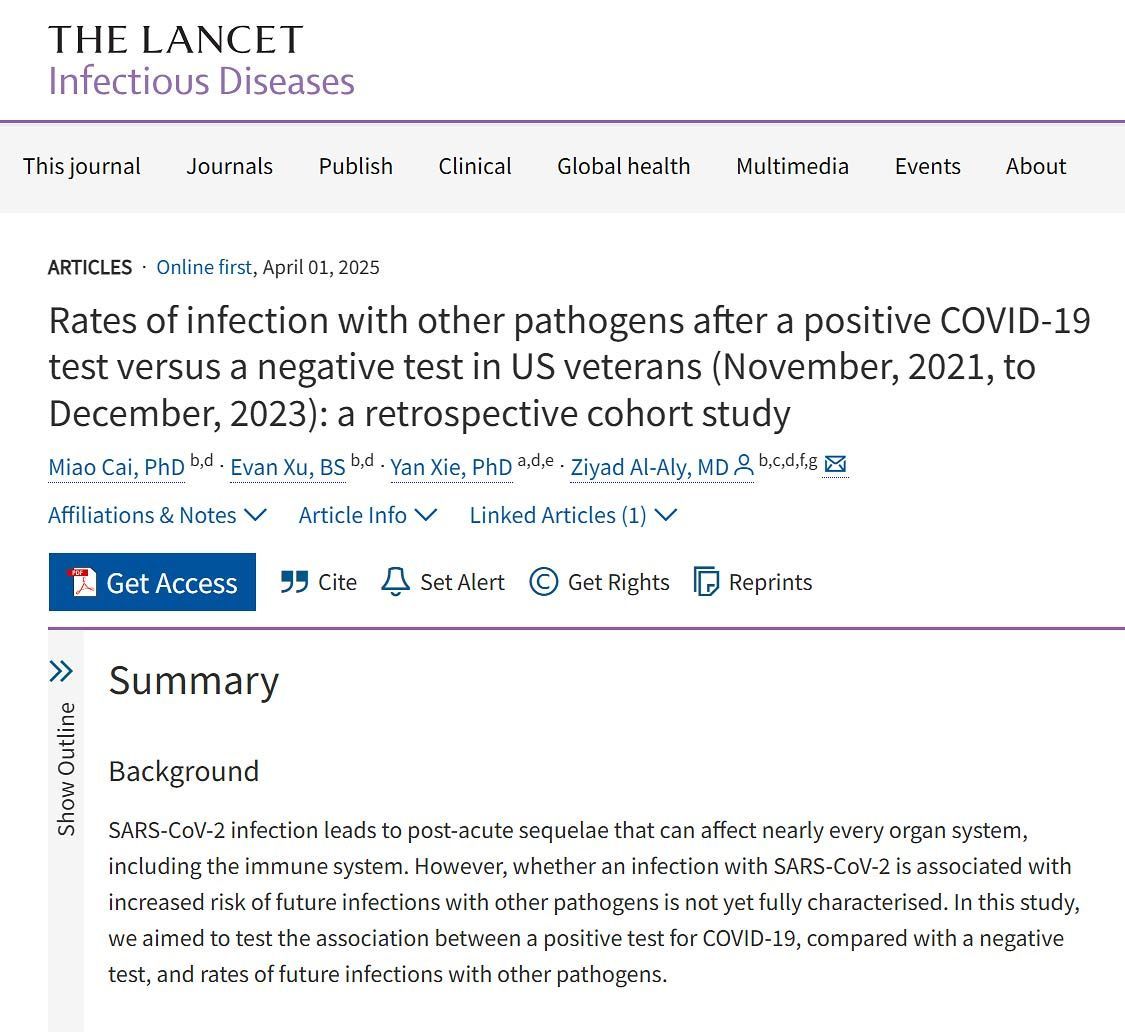
Useful search tags:
air filtration / babies & children / body / brain / C19.Life / cancer / comment / dementia / economy / elders / excess deaths / exercise / flu / heart / history / hospitals / immunity / influenza / law / Lisa Iannattone / long covid / lungs / mitochondria / muscles / musculoskeletal / NHS / Noor Bari / nosocomial / PEM / parkinson’s / propaganda / reinfections / reproduction and pregnancy / resources / respirators / respiratory / risk / SARS(-CoV-1) / schools / solutions / transmission / universities / UVC / vaccines / variants / WHO / young adults / zoonosis